Joint Statement on H.R. 1 by APAMSA, SNMA, LMSA, AMSA, SOMA, and MSDCI
On May 22, 2025, the House of Representatives passed H.R. 1 One Big Beautiful Bill Act, which contained disconcerting provisions aimed at cutting Medicaid funding by almost $700 billion over the next decade. Medicaid has been a central fixture for 83 million Americans, providing essential healthcare and long-term care for children, seniors, people with disabilities, and low-income adults. The Affordable Care Act’s Medicaid expansion to adults who earn up to 138% of the federal poverty level ($21,597 for a single adult) has insured millions of Americans with health coverage. These potential changes will deprive over 10 million Americans from healthcare coverage through Medicaid and disproportionately affect communities of color.
Medicaid has been linked to increased access in rural and disadvantaged areas and improved health outcomes like decreasing all-cause mortality by almost 2% and lowering maternal mortality. In a recent report authored by the Asian & Pacific Islander American Health Forum, the National Association for the Advancement of Colored People, the Leadership Conference on Civil and Human Rights and other national health organizations, Medicaid is the primary source of healthcare for almost 30% of people of color.
Medicaid has consistently enjoyed broad bipartisan support. A recent poll demonstrates that most Americans—Democrats, Republicans, and independents alike—favor maintaining and increasing spending on Medicaid access. Forty states across the political spectrum have opted into Medicaid expansion, recognizing the program’s role in improving health outcomes, supporting rural hospitals, and reducing uncompensated care. Despite the overwhelming evidence that Medicaid is extremely popular across the political spectrum and saves lives, House Republicans have moved to sacrifice public health in favor of funding tax cuts that primarily benefit the wealthy. The harmful provisions in H.R. 1 stand in contrast to the values shared by voters of all political backgrounds who believe Americans should not be denied care due to their income.
The bill will attempt to cut costs by
- Reducing the incentives and federal subsidies given to states for expanding Medicaid, specifically punishing any state that provides any health benefits or assistance to undocumented immigrants with lower expansion matches,
- Establish cost-sharing and copays of $35 for services provided to anyone above the federal poverty level ($15,650 for a single adult),
- Instituting stringent work requirements and eligibility verifications that burdens Medicaid recipients and state governments with more paperwork,
- Prohibiting Medicaid payment to nonprofits and providers that focus on reproductive health, family planning, and abortion services like Planned Parenthood,
- Removing gender affirming care as an Essential Health Benefit under the Affordable Care Act and prohibiting coverage for any Medicaid/CHIP recipient,
- Suspending rules that streamline application and enrollment into Medicaid and for patients who qualify for the Medicare Savings Program (covers Medicare premiums and cost-sharing for low-income Medicare beneficiaries).
We strongly condemn any legislation aimed at limiting equitable access to Medicaid or attacking access to abortion services and gender affirming care. Among the many destructive changes also embedded in H.R. 1, the elimination of federal student loans and loan forgiveness programs will severely limit access for students from all backgrounds to pursue careers in medicine. This bill proposes a lifetime cap of $150,000 for federal graduate student borrowing, specifically for those enrolled in professional programs. This will potentially force students to rely on private loans with less favorable terms and fewer protections, undoubtedly compounding the physician shortages in the very communities that rely on us.
At the heart of these proposed cuts lies an uncomfortable truth – healthcare is not a human right if equal access is not afforded to everyone regardless of socioeconomic class and immigration status. These actions go against the principles set by other nations, the World Health Organization, and the EU among others, highlighting the precarious path that the U.S. government is currently steering the country down. If passed in the Senate as is, the “One Big Beautiful Bill” will greatly harm patients across the United States and hamper the ability for physicians and other healthcare providers to serve their communities.
Call to Action:
To Senators – We call on all senators to reject this bill to protect the American public’s interest and maintain our great nation’s founding principles of “Life, Liberty and the pursuit of happiness”
To Medical Students – we urge all medical students to contact their Senators in Congress and demand a No vote on the “One Big Beautiful Bill.”
Signed,
Asian Pacific American Medical Student Association (APAMSA)
Student National Medical Association (SNMA)
Latino Medical Student Association (LMSA)
American Medical Student Association (AMSA)
Student Osteopathic Medical Association (SOMA)
Medical Students with Disabilities and Chronic Illness (MSDCI)
Additional Resources:
Contact your Congressional Representatives: https://www.congress.gov/contact-us
More information about federal student loans changes: Official Statement and infographic
Call or email your Representative today with a call script from our partner organization, Vot-ER: https://go.vot-er.org/0mAQQu
For questions regarding this statement, please contact:
Rapid Response Director, Brian Leung at rapidresponse@apamsa.org
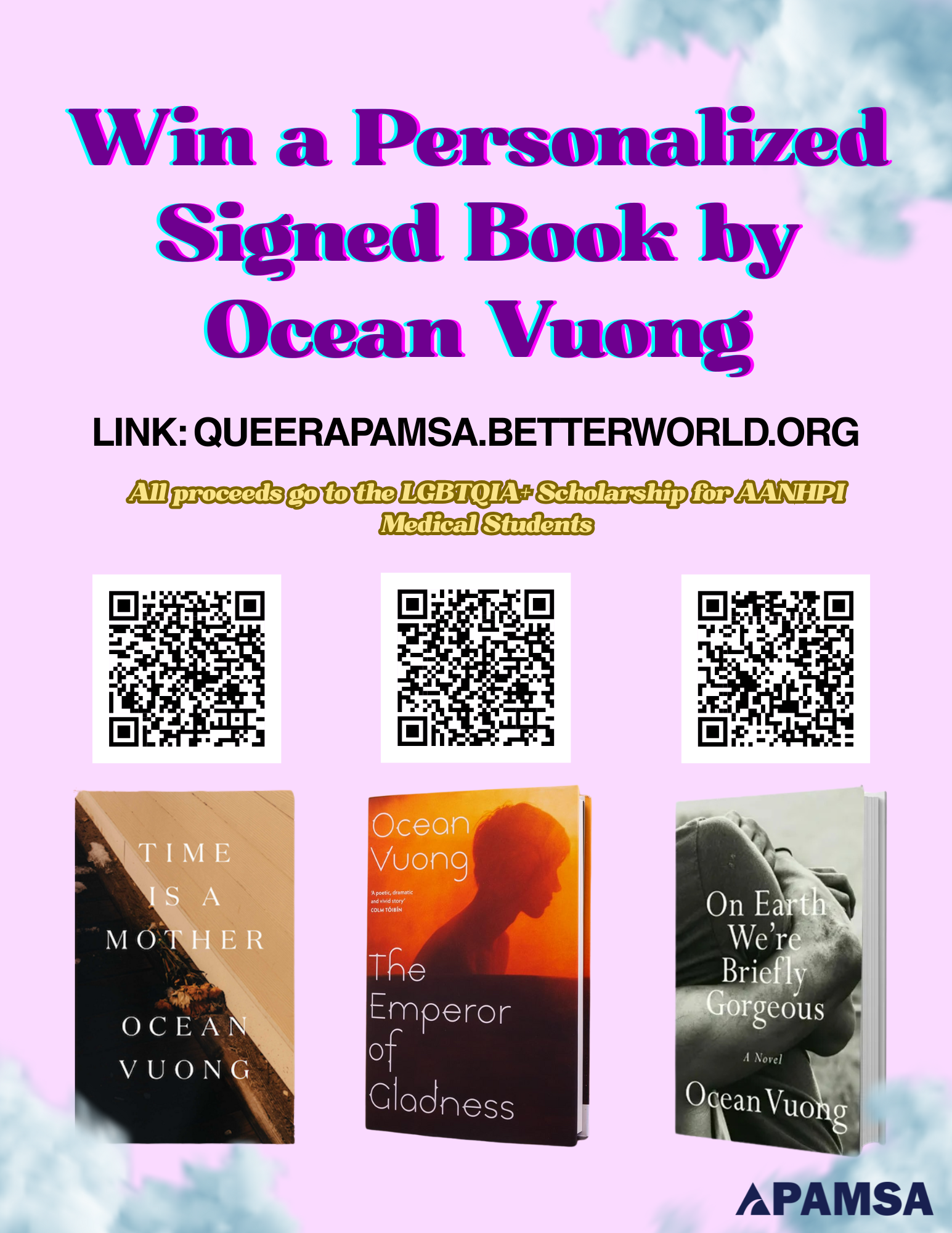
Win a Personalized, Signed Book by Ocean Vuong!
Enter to win a personalized, signed book from Ocean Vuong (unlimited entries!) to raise money for the LGBTQIA+ Scholarship for AANHPI Medical Students!
Three books, donated graciously by Ocean Vuong and his team, are being raffled off: On Earth We’re Briefly Gorgeous, Time is a Mother, and his brand new book The Emperor of Gladness!
Click here to enter!
For questions, please contact our LGBTQIA+ Director, Joey Hua-Phan (he/they), at lgbtqia@apamsa.org
Response to Proposed Limits and Elimination of Federal Student Loans
On April 28, 2025, Congress released a draft proposal to overhaul the federal student loan system, aiming to add limits to federal student loans, eliminate Grad PLUS loans, and drastically scale back current repayment plans and loan forgiveness options. For 75% of medical students who take out federal loans to pay for medical school, these new proposed rules will stifle the training of future physicians in a nation already facing a physician shortage among a growing and aging population. Congress is also discussing changes to reduce Pell Grants, which help fund undergraduate education for low-income students, including pre-medical students.
APAMSA’s membership is made up of over 4,500 medical and pre-medical students from across the country, and our national organization opposes these alarming changes that will irrevocably damage medical education financing for tens of thousands of medical students and for the many other health profession students.
We urge students to spend 5 minutes of their time to reach out to their Congressional representative to demand the protection of federal student loans. Please send this to your fellow classmates – more people contacting means higher importance to our representatives.
To find your Representative and Senators, please use the following website: https://www.congress.gov/contact-us
We have provided scripts that you can use in an email or in a short phone call to deliver your concerns about the proposed changes. Please feel free to adjust these scripts as you wish to better express your concerns. If you have voted for the Congressional representative or senator before, please mention that as a part of your statement.
Version 1:
Hi, my name is [NAME] and I’m a constituent from [CITY, ZIP].
Thank you so much for your continued support of our medical students and the future patients they’ll serve, especially in rural and underserved communities. I’m reaching out today not just as a student, but as someone who grew up in [brief personal background] and who relies on the Grad PLUS program to afford medical school. If this option were taken away, students like me would be forced to reconsider whether they can even afford to complete their training—despite our deep commitment to serving communities in need. I remain concerned about proposals to eliminate Grad PLUS or impose borrowing caps below the true cost of medical education. These changes would severely limit access for students from all backgrounds and risk worsening the physician shortage in the very communities that rely on us. I respectfully urge you to continue advocating for policies that protect access to medical education and ensure that future physicians can continue serving the communities that need us most. Thank you again for your leadership and for considering the impact this would have on students like me.
Version 2:
Hi, my name is [NAME] and I’m a constituent from [CITY, ZIP].
I’m calling to urge [REP/SEN NAME] to protect funding for the federal student loan program and oppose the elimination of Grad PLUS loans and other loan repayment options. As a [medical student/pre-medical student] at [your school], access to federal student loans are crucial to the training of America’s future physicians. In order to provide the best care to our patients across the nation, we must be supported in our education.
Thank you for your time and consideration.
IF LEAVING VOICEMAIL: Please leave your full street address to ensure your call is tallied.
For questions regarding this statement, please contact:
Rapid Response Director, Brian Leung at rapidresponse@apamsa.org
Editor Director, Christine Le at editor@apamsa.org
Director of Organized Medicine, Jennifer Deng at organizedmed@apamsa.org
Statement on Lapu Lapu Day Festival Tragedy
The Asian Pacific American Medical Student Association (APAMSA) extends its deepest condolences to the Filipino Canadian community in the wake of the devastating tragedy at Vancouver’s Lapu Lapu Day festival. On April 26, 2025, a vehicle was driven into a crowd celebrating Filipino heritage, resulting in the loss of 11 lives and injuring over 20 individuals.
This senseless act has left an indelible mark on a community that was gathered together in joy and cultural pride. As future healthcare professionals committed to serving Asian American, Native Hawaiian, and Pacific Islander communities, we stand in solidarity with those affected. We honor the resilience of the Filipino community and the dedication of the first responders and healthcare workers who provided immediate care and continue to support the victims and their families.
APAMSA reaffirms its commitment to fostering safe and inclusive environments for all communities. We pledge to advocate for mental health awareness, community support systems, and preventive measures to ensure such tragedies do not recur (Resolution 30.001). In this time of mourning, we offer our support and stand united with the Filipino Canadian community.
For more information on how to help, please look to Filipino BC (@filipino_bc) and at the official City of Vancouver website for more updates and ways to support the community in the future.
If you or someone you know needs support, please reach out:
988 Suicide & Crisis Lifeline: Call or text 988 (24/7, nationwide)
Asian Mental Health Collective – Resource Directory: asianmhc.org/resources
Crisis Text Line: Text HELLO to 741741
For questions about this statement, please reach out to the National President, James Chua at president@apamsa.org, the Southeast Asian Director, Fern Vichaikul at sadirector@apamsa.org, or the Rapid Response Director, Brian Leung at rapidresponse@apamsa.org.
APAMSA Merchandise Order Form: Graduation Cords
Response to SAVE Act (H.R. 22)
On April 10, 2025, the House of Representatives passed H.R. 22, the Safeguard American Voter Eligibility (SAVE) Act, which requires all voters to provide documented proof of citizenship in person while voting. If passed in the Senate and signed into law, this bill will create unnecessary barriers to voting and disenfranchise millions of eligible voters.
| Parts of the SAVE Act | Who does this impact? |
|
One in 10 eligible American citizens lack these documents or face significant barriers in obtaining them.
Voters of color, married women who change their names, and young voters will be significantly affected. Those with REAL ID, military or tribal ID would not be considered as having sufficient proof of citizenship under this new law. |
|
Every current and new voter will have to present their proof of citizenship to election offices, which can be hours away, in order to update their registration status. This poses a significant burden for rural, disabled, and elderly citizens.
This also eliminates voter registration drives and online voter registration, thus reducing voter turnout. |
|
Voting as a noncitizen is already illegal and very rare – only 30 votes out of 23.5 million votes during the 2016 general election were suspected to be made by noncitizens.
During previous voter roll purges, almost two-thirds of suspected noncitizens in Alabama were, in fact, later found out to be eligible voters. If rolled out on a larger scale, this will unjustly disenfranchise eligible voters as already seen in Virginia during the 2024 election. |
National APAMSA strongly condemns this bill, as it will have far-reaching effects in limiting the voices of millions of Americans, especially people of color who are disproportionately affected by this potential voting law. We stand by the statements put out by organizations like ACLU and APIA Vote that echo our same concern for diminishing voting access. As mentioned by previous statements, National APAMSA recognizes that voting is a pivotal social determinant of health that underlies our ability as medical students, health advocates, and future leaders of health to serve our communities and strive for better health outcomes.
Please contact your local Senator to express your opposition against the passage of the SAVE Act. You can use 5 Calls to quickly locate your representatives’ numbers and be prepared with prompts that can help you discuss this particular bill and other issues at ease. Other resources like When We All Vote can also streamline the process to contact the appropriate representatives.
For questions or concerns, please reach out to Brian Leung at rapidresponse@apamsa.org
Response to Executive Order to Eliminate the Department of Education
On March 20, 2025, President Donald J.Trump signed a new executive order directing the Education Secretary, Linda McMahon, to pursue the closure of the Department of Education (ED). The ED distributes over $1.6 trillion in federal loans and financial aid for students, enforces civil right laws such as Title VI and Title IX, funds public school budgets, and gathers education statistics. The executive order also directs the Education Department to restrict any federally funded programs or activities under the label of “diversity, equity, and inclusion (DEI),” reinforcing previous executive orders aimed at rolling back DEI initiatives.
Given that over 70% of medical students take out loans, especially utilizing federal loan programs like the Direct Unsubsidized Loan or Graduate Plus loans, the closure of the ED will jeopardize these loan programs and loan repayment programs that have been a cornerstone reducing medical education debt.
National APAMSA condemns this policy directive that will undermine student education funding and diminish the protections against racism and discrimination in schools and colleges across the nation. As mentioned in our previous statements and in our official policy compendium, APAMSA continues to advocate and work with policymakers and professional organizations to protect efforts to increase diversity and equity in medical education.
We urge Congress to oppose any bills aimed at formalizing the elimination of the ED and to commit to the protection of the department and countless other diversity programs. Please contact your local Congressional representative to express your support to maintain the Department of Education.
For questions about this statement, please reach out to Brian Leung at rapidresponse@apamsa.org. For local support, please contact your regional director.
For questions or concerns, please reach out to Brian Leung at rapidresponse@apamsa.org
Response to Government Censorship of LGBTQIA+ Health
On January 20th, as part of President Donald J. Trump’s day-one executive orders, the Office of Personnel Management directed federal agencies to eliminate “gender ideology” from employee resource groups and grants and replace the term “gender” with “sex” on government forms. As a result, vital public health information and data have been erased from the Centers for Disease Control and Prevention website, including HIV testing information, the Social Vulnerability Index, contraceptive eligibility guidelines, the largest adolescent behavioral health monitoring program, multiple resources addressing health disparities among LGBTQIA+ communities, and more.
National APAMSA denounces the draconian censorship of science, public health, and medicine in federal policy to further disenfranchise marginalized communities. Regardless of federal mandates, we will continue to advocate for the dissemination of evidence-based, culturally competent care and support initiatives that combat health disparities among sexual and gender minorities. We affirm that gender-affirming care is life-saving care, as discussed in our previous statements and policy compendium, and affirmed in the stances of the World Health Organization, American Academy of Pediatrics, American College of Obstetricians and Gynecologists, and American Academy of Family Physicians.
We urge all healthcare professionals to adhere to the evidence-based clinical recommendations and guidelines that have ensured quality care for all communities. We urge institutions to support their employees and patients by continuing to ensure diversity, equity, and inclusion in their resources and programs. Lastly, we urge community leaders and policy makers to prioritize the health of the public and act against censorship of medical terminology and public health institutions.
To our colleagues in medicine, we stand with you and fight alongside you. We affirm that diversity is what makes our communities strong.
To our patients, please know that there is an overwhelming majority of healthcare workers that will fight to provide the highest level of care possible. Please continue to share your stories and seek the care you deserve. It is our highest honor and privilege to care for you and your loved ones.
“It is in collectivities that we find reservoirs of hope and optimism.”
― Angela Y. Davis, Freedom Is a Constant Struggle
For questions about this statement, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org. For local support, please contact your region director. To get more involved with National APAMSA’s diversity initiatives, please visit www.apamsa.org/diversity or contact Sandra Kumwong at diversity@apamsa.org.
For questions or concerns, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org
National APAMSA Statement on President Trump’s Day One Executive Orders
On Monday, January 20th, President Donald J. Trump issued a slew of executive orders disrupting public health and safety, including actions related to health care, Covid-19 and emergency preparedness, diversity, equity, and inclusion, LGBTQ+ protections, immigration, climate change, reproductive rights, and the death penalty.
National APAMSA condemns these overwhelmingly unconstitutional policies aimed at disempowering marginalized communities. As discussed in previous statements and our policy compendium, we will continue to uphold health care reform; protection of migrants, refugees, and undocumented immigrants; and advocacy in favor of dismantling racial, ethnic, and gender disparities.
While these recent events may be discouraging, we encourage our community to practice resilience, center optimism, and remain energized. In memory of Martin Luther King, Jr. this week, we offer a reminder: “We are now faced with the fact that tomorrow is today. We are confronted with the fierce urgency of now. In this unfolding conundrum of life and history, there ‘is’ such a thing as being too late. This is no time for apathy or complacency. This is a time for vigorous and positive action.”
We urge community leaders, lawmakers, and judicial systems to challenge these executive actions and fight for justice, equity, and inclusion for all. Find and contact your representatives in Congress by visiting www.congress.gov/members/find-your-member.
For questions about this statement, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org. For local support, please contact your region director.
For questions or concerns, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org
Response to Police Assault of Lich Vu
On October 27, 2024, 71-year-old Lich Vu was brutally assaulted by police during an arrest in Oklahoma City, which resulted in severe injuries requiring hospitalization. Body camera footage released by the Oklahoma City Police Department reveals a language barrier between the officer and Vu, who is Vietnamese and speaks English as a second language. The incident brings to light dual issues of police brutality and increased violence against Asian American, Native Hawaiian, and Pacific Islander (AANHPI) communities in the wake of COVID-19.
National APAMSA strongly condemns the assault on Lich Vu and reaffirms our stance against police brutality and violence against AANHPI communities, as discussed in previous statements. Police violence is not only a criminal justice issue, it is also a public health crisis. The immediate physical harm inflicted in such incidents is accompanied by long-term psychological and emotional consequences, not only for the individuals directly affected but also for their families and communities. For elderly individuals like Vu, these effects are compounded by the vulnerability that comes with age and the challenges many immigrants face in navigating systems that often fail to protect them.
The health of our communities is deeply intertwined with how institutions like law enforcement uphold—or undermine—public safety and trust. Yet, these harms are preventable, and addressing them requires systemic change. Accountability must be pursued at every level to ensure justice and to prevent similar incidents in the future.
Our thoughts are with Lich Vu and his loved ones as they recover from this traumatic event. We continue to urge community leaders, policymakers, and law enforcement agencies to take decisive action to ensure accountability and enact reforms that prioritize the safety and dignity of all individuals, especially the most vulnerable among us.
Written by Hugo Zhou and Nataliyah Tahir.
For questions or concerns, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org