Response to Police Assault of Lich Vu
On October 27, 2024, 71-year-old Lich Vu was brutally assaulted by police during an arrest in Oklahoma City, which resulted in severe injuries requiring hospitalization. Body camera footage released by the Oklahoma City Police Department reveals a language barrier between the officer and Vu, who is Vietnamese and speaks English as a second language. The incident brings to light dual issues of police brutality and increased violence against Asian American, Native Hawaiian, and Pacific Islander (AANHPI) communities in the wake of COVID-19.
National APAMSA strongly condemns the assault on Lich Vu and reaffirms our stance against police brutality and violence against AANHPI communities, as discussed in previous statements. Police violence is not only a criminal justice issue, it is also a public health crisis. The immediate physical harm inflicted in such incidents is accompanied by long-term psychological and emotional consequences, not only for the individuals directly affected but also for their families and communities. For elderly individuals like Vu, these effects are compounded by the vulnerability that comes with age and the challenges many immigrants face in navigating systems that often fail to protect them.
The health of our communities is deeply intertwined with how institutions like law enforcement uphold—or undermine—public safety and trust. Yet, these harms are preventable, and addressing them requires systemic change. Accountability must be pursued at every level to ensure justice and to prevent similar incidents in the future.
Our thoughts are with Lich Vu and his loved ones as they recover from this traumatic event. We continue to urge community leaders, policymakers, and law enforcement agencies to take decisive action to ensure accountability and enact reforms that prioritize the safety and dignity of all individuals, especially the most vulnerable among us.
Written by Hugo Zhou and Nataliyah Tahir.
For questions or concerns, please reach out to Nataliyah Tahir at rapidresponse@apamsa.org
Open Positions for 2025-2026 APAMSA National Board
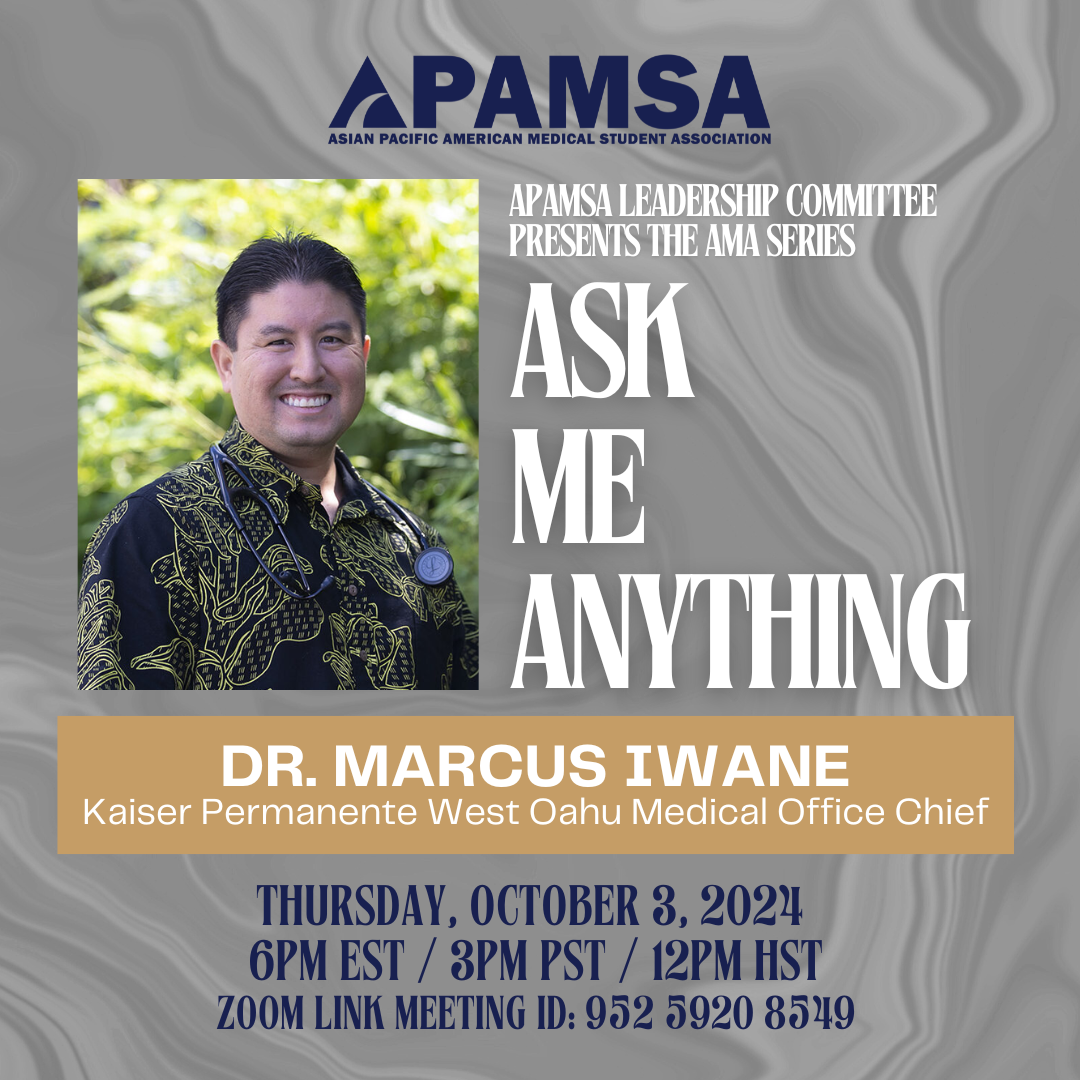
CALLING FOR CANDIDATES to run for the 2025-2026 National Board!! We have a few Round 2 positions that are available for you to run for:
External Affairs Branch:
Sponsorship Directors
Fundraising and Scholarship Director
Communications Branch:
Network Director
Editor Director
Health Affairs Branch:
Community Outreach Director
Bone Marrow Director
Strategy Branch:
Alumni Directors
Pre-Health Directors
Diversity Branch:
Hawaiian and Pacific Islander Director
Southeast Asian Director
LGBTQIA+ Director
Membership Branch:
Region 1, 2, 3, 4, 5, and 8 Directors
Link to apply: https://forms.gle/8jiZVWCGSJiEFEem9
For full details, visit our website at apamsa.org/elections.
A Conversation With Donna Tran

Listen here:
YouTube
Spotify
Apple Podcasts
This episode was produced by James Chua and Ashley Tam, hosted by James Chua, and graphic by Callista Wu and Claire Sun.
Timestamps:
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
00:24 Introduction to Donna Tran
02:40 Doctor Who and Drag Queens
07:57 Getting Involved in Health Policy
13:11 The Inspiration for Medicine and Advocacy Work
16:35 Why Psychiatry?
20:39 Learning About and Joining APAMSA
25:04 Donna’s APAMSA Legacy
30:32 Debunking Misconceptions of the Medical Field and School
37:07 This Or That? Questions
41:20 Advice for Pre-Health and Medical Students
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
James: Welcome everyone to the fourth episode of the APAMSA podcast. From roundtable discussions of current health topics to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization, this is White Coats and Rice. My name is James Chua, second year medical student at Tour University, Nevada, and the current fundraising director here at APAMSA. And I’ll be your host for today.
00:24 Introduction to Donna Tran
James: On today’s episode. We’re very excited to welcome our first APAMSA alumni guest, Dr. Donna Tran, an inspiring leader in medicine, health policy, and the AANHPI community. A proud daughter of Vietnamese immigrants and a native of San Jose, California, Donna’s journey to medicine refelcts a deep commitment to service, advocacy, and innovation. Donna completed her undergraduate studies at UC Davis, post-bacc program at CSU East Bay, and earned her medical degree at Michigan State University College of Human Medicine. Additionally, she also earned her Master’s of Public Health from Johns Hopkins University. Her impressive career spans public health and federal policy work, including internships with both the US Senate and House of Representatives, as well as a collaboration with President Biden’s Advisory Commission on Asian Americans, Native Hawaiians, and Pacific Islanders. Donna has also served as an appointed commissioner for the City of San Jose’s Senior Citizens Commission. From 2021 to 2023, Donna served as the national president of APAMSA, leaving a lasting legacy through her tireless dedication to amplifying AANHPI voices and creating opportunities for community engagement. Now, a PGY-1 intern, she continues to advocate for health equity and cultural competency in medicine. Outside of her professional achievements, Donna is a proud dog mother to a French bulldog named Boba Princess, seeks to reach new heights not only in medicine, but also with climbing and bouldering, and is a culinary expert, which is distinguished by a Yelp Elite Black Badge. Without further ado, join us as we explore Donna’s incredible journey in medicine, her insights on leadership, and the unique passions that shape her inspiring story. Donna, welcome to the podcast. How are you doing today?
Donna: I’m doing well thank you, just enjoying the last bit of sunlight during Winter.
James: Yeah, absolutely. And a lot of that came from your many bios on the APAMSA website. Yeah, so if it sounds familiar, that’s where it was all taken from
Donna: I’m very complimented, thank you.
02:40 Doctor Who and Drag Queens
James: No, we are just so like, we are so excited to have you as our first alumni. Like your story is just so interesting. And I imagine that there are plenty of doctors that have inspired you throughout your time and probably have made you the doctor that you are today. I can probably think of like Dr. B Li or Dr. Jhemon Lee, just to name a few. But there is one doctor I’m very interested to know, like how they have inspired you and that is Doctor Who.
Donna: Oh, oh my gosh, I’m flabbergasted right now. Yes. Doctor Who. I actually got into it because my cousin and my brother started watching the 10th Doctor, David Tennant, back when he first came out in the early 2010s. I’ve heard of Doctor Who. I was like, “Oh, this is some weird British sci-fi thing.” Then they’re like, “Oh yeah, just watch an episode with us.” Then I just got totally hooked. So this was before med school. I actually went to Silicon Valley’s Comic Con and David Tennant was here in San Jose area and I had to pay like $100 to get like a picture taken with him and his autograph. And I told him this was like when I was applying to med school I was like oh yeah I’m like going to medical school like Doctor Who was like you know your characters inspired me so much into becoming like, kind of doctor I wanted to be. And he like, perked up and he’s like, “Oh, brilliant”. And I was like, oh, my god, it was the best moment of my life. So yeah, so I met him in person. He’s amazing. He’s really nice. Like, even though, you know, like 1000 fans are like, going through and taking pictures with him, but he is still my all-time favorite doctor. Doctor Who is still going on now. Give it a watch. Yes, it’s a huge time investment, but I just think it teaches me so much about character in such a good sci-fi sense versus Game of Thrones, which I also love, but it’s like very messed up. So I feel like it’s at least more like nerdy hopeful positive. So yeah, I still watch Doctor Who and I love it so much.
James: Have you? So you still keep up with the most recent seasons of Doctor Who then, ya?
Donna: Yeah. Yes. I know the most recent one was Ncuti, the black doctor, and I haven’t seen the whole thing yet. I know there was a Christmas special that just came out so I have to catch up. But I’ve like caught up like like with the ninth doctor, 10th, and then 11th is Matt Smith, which I think most people know by association of his face. And then you have the 12th doctor, which is an old dude, 13th was a woman, I think her name was Jodie Whitaker. And the 14th now is Ncuti.
James: I think the 12 doctor is Peter Capaldi, right?
Donna: Thank you. Yes, Peter Capaldi. Thank you. Yeah.
James: I’m somewhat familiar with Doctor Who. I remember back in my younger years when I used to be on Tumblr, I would always see Doctor Who content all the time.
Donna: Oh memes! Memes upon memes!
James: But I really, it’s so, you know, warming, especially for me, personally, as like a queer person to see like how inclusive Doctor Who can be. And especially, that’s why I was curious if you’re keeping up with the latest season because to my knowledge they have not only drag queen but non-binary actor Jinkx Monsoon is one of the um…
Donna: Oh I love Jinkx! Yes. Yes. I haven’t, no I haven’t seen their episode yet but I also used to watch RuPaul’s Drag Race and I definitely did watch Jinkx Monsoon’s season. But don’t quote me on anything. I just don’t remember anymore but I do know some of the drag queens, they’re amazing.
James: Yeah, of course. And I feel like, that is such an important thing, like the sense of inclusivity. And I also watched a lot of drag race. I think one of my personal biggest accomplishments prior to me joining APAMSA, and I think it sor of led to like why I work towards serving the communities that I do, you know? But um, back in the day when I was at, uh, my undergraduate university, it was the University of San Diego and to our listeners or to you, if you didn’t know, that is a private Catholic institution.
Donna: Oh- I did not, isn’t that the party school?
James: No, that’s San Diego State University.
Donna: Oh, state, thank you. Okay, got it.
James: Yeah, I get that a lot. It’s either, oh, you went to UC San Diego, and I’m like, no, that’s the La Jolla School, and then they’ll be like the party school. But in any case, what I’ve been meaning to say is that, back when I was an undergrad, one of the things that really ruffled a lot of feathers was we hosted a drag show on campus, you know, to amplify queer voices and we would always invite drag queens to host the show, you know? And one of the amazing queens we got to bring through to host the show was Bob the Drag Queen before she won her season.
Donna: Stop! You met Bob? What?! That’s amazing!
James: They wore the dress they made from the first episode of their season.
Donna: They’re a legend. Yeah. Even I know Bob. Yep.
07:57 Getting Involved in Health Policy
James: Yeah. But one of the things that I think is particularly special about Bob the Drag Queen that you parallel is how politically involved they are. You know, and I would love to hear more before we dive deep into your journey through medicine. Like what inspired you to do so much policy work? I feel like they’re – for at least for me, so I don’t want to speak for everybody. But I find that there is such an overlap between medicine and policy. But for a lot of folks, they don’t know how to, you know, if they have a passion for both legislation and medicine, how to incorporate the two. And so to see how much you’ve done, like it’s so inspiring and so how did you get started on that?
Donna: Yeah. So this is going to sound funny. But I used to be like not interested in politics at all. I used to be borderline apolitical prior to med school. I knew that there were elections. I knew Obama won and Bush won before. But I just didn’t, and I don’t know if that’s like an age thing, but when I was younger, I was just very so much in my bubble. And I didn’t know exactly what the three branches of government did years ago and I think medicine comes hand in hand with being involved in the community and advocacy. Like, it’s difficult to remain in that bubble as you progress through your medical journey without opening a few eyes and a few doors. And the reason why I say that is because I knew in med school I – I was obviously happy with the clinical training we getting, that’s what med school does, it pumps you up as a doctor, but I was not happy with what I was taught in terms of population health, in terms of how we can help communities, what does that system look like you know, that’s, you know, beyond your school. And so I actually chatted with the California Surgeon General Dr. Diana Ramos a few months ago, and she told me a really good quote that I still remember to this day. She said that “80% of healthcare happens outside the four walls of your exam room.” And I 100% believe that. And the reason is because if you have patients who can’t afford medications, who can’t afford treatments, who have a very poor diet, they’re in a food desert, right? All of those things contribute to them coming back to see you all the time in the hospital right? Readmission rates are high, etc. And so for me, I wanted to get that experience. And so I wanted to get an MPH and that’s when I started getting a little bit more like learning about politics and about like advocacy, and it really didn’t click for me until I was like in that scene. So when I went to Hopkins, it’s in Baltimore, which is literally across from DC. And really just a geo-like political landscape and opportunities that were there. I was like, you know, I should toss my hat in the ring and like apply for these internships and see where I land. And so I think and I say this to a lot of people all the time, like, “Yes, I’ve had a long CV, but I have probably three times the number of applications and twice the number of rejections.” So nine out of 10 things I apply for, I get rejected from. And that one thing that I applied for and that I did get, I try to learn something from that, or I stick with it and I try to be really good at it. And so for me, wanting to be in that advocacy scene, one, you need to place yourself where the action is. You can’t just say like “I want to learn about this, but I’m just going to sit here and, and read, read”. Reading is great to get knowledge, but if you’re not out there being in, you know, positions of power or getting leadership experiences, it’s not going to help you and it’s not going to help anyone else. And so I think during my APAMSA term, and even now, trying to create a physician organization for Asian Americans, I still have the same mindset. Is to give opportunities, to raise awareness so people can be leaders themselves. So thats the first part, and then I think the second part is just not giving up. And why I say that is because I actually was City Commissioner, like you mentioned when I was actually a med student. I was a fourth year med student and I was a City Commissioner. Not that I Googled who else was, but I would probably soundly say not a lot of people did that, their fourth year med school and I just applied for it. I applied for it on the city of San Jose’s commission board website. It looks like a website from the 90s. I wasn’t even sure if my application was going to some black hole and then my council member called me and said, “Hey congrats, we’re going to appoint you as City Commissioner” and I was just a med student. So never feel like, you know, you can’t do something based on the level of where you’re at, you can do anything at any time. And so those are probably like the two things that I’ve learned on my journey so far in terms of like marrying medicine and advocacy.
13:11 The Inspiration for Medicine and Advocacy Work
James: Truly we don’t have the cameras on right now, but my mouth is a gape. That is so like inspiring to hear. Wow. Would you say your journey in policy work has closely paralleled your career, like the beginnings of your medical journey? Like, so in other words, I’m asking like, how, where did your journey in medicine begin, you know, and how closely did that tie to policy work? If there even is an overlap in the genesis of the Donna Tran medical journey.
Donna: Oddly, I would actually say actually the medical journey began a lot earlier than my advocacy political journey. And that’s because, you know, years ago, my father, my whole family is like OG immigrants. I was born here but they came over like during the Vietnam War. And my dad, long story short, had a brain tumor, was very like, anti feelings, anti mental health, and that just took a toll on our family. And I live in, we’re from San Jose, California, where there’s like a huge number of Asian Americans in general, and just, they just could not find an Asian therapist. It was actually very shocking. Even today if you look at like the AAMC workforce data. There’s, you know, from last year to this year, last year’s Asian physician workforce was 18% and this year was 19%. And sometimes those numbers just don’t make any sense for certain communities that have such a high number of Chinese Americans or Hmong Americans, and there are not enough physicians to serve them. And I’m like literally in Silicon Valley. So I can’t even imagine what a physician desert it is in some areas across America. And so in general, I would say that kind of kick started off my journey in exploring medicine and how I can help families in those areas and similar situations. And then after that, I think the political and advocacy work came a lot later, ’cause I was just like, focused on getting into med school, doing well on my MCAT. When you look at people’s CVs, you’re like, “Oh, wow, they did a lot of things.” I don’t know. At least on my end. I was like very like like one step minded. I was like I gotta get to like post-bacc I gotta get to medical school and then now I’m in residency. And I didn’t believe it like previously but when I would ask leaders the same question like oh, how did you get involved? Or you know how did you get all these opportunities there like number one answer was serendipity and I just would not believe them. But now I get it, I totally get it. You know, you have, like I said, you have to put yourself in places and situations and try to like figure it out like what you’re really passionate about and then just kind of take each experience as it comes along and learn for that. So the advocacy part, I’m still trying to figure it out now. Um, and it’s more advocacy than political. I don’t have any desires right now to run for office. Um, I worked with politicians and it’s, it’s a lot, it’s a lot of hard work. So if you want to run for office, I’m more than happy to help run your campaign. But I’m very happy with doing legislative stuff on my end.
16:35 Why Psychiatry?
James: Yeah, absolutely. And so something I want to dive a little bit more deeper into and it’s another reason why I look up to you as a role model, but you were touching, talking about earlier about mental health, especially amongst like immigrants, Asian immigrants. It’s not discussed as much as it should be. And you know, and that unfortunately trickles down to our generation, you know, as first generation American, Asian Americans, you know. Did that – That must have played a major role in you choosing psychiatry. So I’m ask- so what I’m asking is, at what point did you realize, like, you know, psychiatry is the one for me? How did your upbringing or how did your background like sort of lend to that?
Donna: Yeah, so I would say, um you know every so every med student uh is going to go through third year rotations, psych is one of them. When I went through my psychiatry rotation it was the best ever. One, because a lot of things that we helped patients with were very personal and intimate, and medicine is already intimate enough, but to explain this further, when I was in my surgery rotation which is– people think are like polar opposites, right, surgery versus psychiatry. When I was in my surgery rotation they were like in awe. They were like, “oh, you’re interested in psychiatry, we’ve had some we’ve read some psychiatry colleagues actually become psychiatrists and we were trying to figure out like the correlation between them and what we kind of figured out was that with surgery, you’re basically cutting into a person right like you’re sticking their hand into their abdomen. That’s as pretty physically intimate as you can get. Right? Like you’re literally cutting into a patient and sewing them up. For psychiatry, you’re basically doing that, but you’re dissecting their mind. And you’re figuring out their traumas, like what it is that they really think, what drives them as a human being. A lot of my co-interns really like this philosophical view on psychiatry as well. It’s more of a narrative medicine. And so I think that, you know, after going through all of my rotations, like, this is the one for me. I want to figure people out. I want to figure out how to help them, because you know like there’s a pill you know for diabetes and yes there are pills for depression and stuff like that. But if you ask any psychiatrist, no one is going to give you a straight answer on exactly how to fix depression. There is no definitive or numerical answer, right? Versus like diabetes, you have a hemoglobin A1C, like either you have diabetes or you don’t, right? Pretty easy. With depression or like schizophrenia the other psychiatry like um, diseases and disorders, it’s not that straightforward. And so I kind of like that complexity, and I find that incredibly rewarding. And a lot of public health is a lot of public mental health as well. Behavioral things that people can do to increase not only their mental health but also their physical health too. And so I think that right now, in the past few years, since the pandemic started in 2020, mental health has kind of exploded on the scene. You know, everyone’s just now paying attention to it a lot more than it used to be and telehealth is basically rising in the ranks. And so just you know, having followed along this past like four years, I think, it’s been really interesting to see how psychiatry evolved as a field and also in the landscape of medicine. So I’m very interested to see in this upcoming administration, how psychiatry medicine is going to be impacted by this different you know presidency this different congress right it’s going to be completely Republican run, and seeing like what that does to medicine and our population health in general?
20:39 Learning About and Joining APAMSA
James: Yeah, absolutely. That is um…I there’s so much. Yeah. I can’t even imagine how. Cuz we don’t really think about the environmental factors and how they impact, you know, our mental health. Environment, meaning like anything not like out of our control. Man, that is a very wild thought to ponder, you know? And so you talk about how your third year rotation is when it clicked for you for psychiatry. If we rewind just a little bit more, was it your first or second year that you joined APAMSA?
Donna: Oh, joining APAMSA was actually a wild, another wild story. So, I don’t know. I always laugh at this because I don’t know if it makes me a good president or a bad president before, but before like med school, I didn’t really know APAMSA existed. Like, when I got to med school, I was like, “Oh, it was probably like some Asian med student organization,” and that’s when I found APAMSA. But literally like did not exist until like med school. So I like first semester of med school we had some really nice upperclassmen, second years. I think they went to the 2018, 2019? Like that National Conference. It was in person, it was pre-COVID in person. And they were like, hey, we need some like regional director who wants to run and like, no one was running because it was the Midwest. Like, no, there was like one, not enough like representation, which was sad, but also two like, I’m telling you, like people, like, for some reason, like, don’t want to run for positions or don’t want to have these experiences. It’s wild for me. So me and a couple of my classmates ran for RD, regional director positions, and we got it because no one else ran for it. And so that was my first way into like being involved with APAMSA. And then luckily, for me, someone, another national board member was unable to finish out their year as Committee Outreach Director. And so I was the very last person to actually hold two national director positions at the same time. And I thought it was going to be like crazy. I’m a very yes-hype woman. So I was like, oh, yeah, totally. Like I’m happy to help out. But it turned out okay. I think because of those two experiences simultaneously, I got to talk to different branches, different people in APAMSA and I loved it. Then I ran for EVP and then President and the rest was kind of history. But yeah, I started very early on and stayed involved because I think the people that you meet, the friends that you meet, they’re still my friends now. Like I literally text them like almost every week. So if APAMSA is a wonderful organization, I think I’m preaching to the choir here, but and everyone truly wants to make a difference, you know? And I think that that’s what really drives people to be in APAMSA and to stay together.
James: Yeah, absolutely. I think in my own experience, since I’m now only I’m barely about to have one year of APAMSA national board under my belt, I will say for anybody that is interested like, to our listeners who may be interested in running for the national board. If you do decide to pursue this opportunity, it will really change your life, but it is what you put into it, you know? You could just let this just be a residency builder for med school or to get into residency. But like, so far, all of my favorite memories have been the ones where I created events or I collaborated with others and made everything a united effort. You know, this, for example, like I mentioned this in the introduction, like I’m just the Fundraising Director. You wouldn’t expect–
Donna: You’re not JUST the fundraising director. You’re our fundraiser, you’re THE fundraising director. Yeah.
James: True, true, true. But you wouldn’t necessarily expect the Fundraising Director to be the host of the APAMSA Podcast, you know? But it’s about taking your unique skills and sharing it with the organization and allowing you to flourish in the most beautiful kinds of ways, you know?
Donna: Yeah, I agree. Absolutely.
25:04 Donna’s APAMSA Legacy
James: And so in your case, you know, since you’ve served, like you’ve worn so many hats, you’ve done so many things for the organization, looking back, what are some of the things you are most proud of during your time in APAMSA?
Donna: Yeah, I think what I’m most proud of was, I found my purpose and I stood by it and I still stand by it, it’s actually my purpose. And I think from that very cemented purpose came like, you know, multiple initiatives that I wanted to start and are still in effect today. And so, you know, my, I think that everyone, they have the potential to be a leader. And it really just takes a little bit of awareness, a little bit of opportunity and some magic. And I think that everyone can find a place within our healthcare system within this world to be able to enact the changes that they want to. So I don’t think, you know, APAMSA being on national board or executive board is like this exclusive elite club. It absolutely is not. Everyone came from somewhere and I’m very humbled by that belief that I hold every single time. I don’t think anyone is too big or too small for a task. I like still make PowerPoint excels, right. Like, I don’t have a secretary doing that for me. But really, like leaders just start out, you know, doing things that they want to help solve problems and help the community with. And so because of that belief that I had, I really tried to instill that into my national board during the two years. And so there were some things that I wanted to implement that would sustain the organization for a very long time and be able to carry on you know these like legacy aspects of that that would help future students as well. And so one being give you an example was membership dues. We were the student medical student organization to not like have membership dues. And I think in part was because we’re a newer organization we started around 1994. And so, you know, you know, a lot behind many years behind you know, SNMA or LMSA, but that’s totally fine right come in existence when we come, but at the same time, we were also struggling to keep afloat, to be able to do all these initiatives and support our students with grants, scholarships, etc. So one was implementing dues. And the second thing was creating more opportunities and structure within national board to be able to pipeline just, you know, student members who want to explore the national board and come into these positions of leadership. For example, when I just started into my presidency, we actually created the diversity branch. You would think that it was here forever but it was not. It is like maybe five years old. It’s not that old. Same with advocacy. Advocacy just came into existence right before I got into the National Board. It was like probably within like 10 years old or something like that. So Diversity branch was created, we created also multiple committees nationally standardized National Committees for the Diversity branch. So in addition, like created like the Leadership position Director, Women’s Director position, and created those like corresponding committees as well. So all these things is to increase participation, engagement, and I just really wanted to nail in that you know, this isn’t like a me position, this is a we position. I cannot run everything by myself as president during that time, no matter how much you think you can, but it needs to be a team effort. And so I think that me trying to instill those values and seeing some of those initiatives still be in existence today, it still makes me very proud. So good job guys. I’m not doing any of those work anymore. You all are. But you know, just being able to recognize that, you know … in a place temporarily and how much good we can do is really reflected on what you can leave behind that’s sustainable and that is positive. And so every though I’m a resident now like I still always come back because the APAMSA so was so much fun and it was so meaningful that I think that you know, it was really such a rewarding experience for me.
James: Absolutely. I mean you truly do have such a long-lasting legacy at APAMSA. I think something that inspires me so much about the work you’ve done and so much of the national board and past presidents and everybody, all of the alumni, is that like, what you guys have done is truly like. You found APAMSA in a away and then you left it in a better state than what you got.
Donna: We tried.
James: And so that’s, I feel like if somebody is ever interested in joining this org, that’s what should be motivating them to do more than what their position entails. What can you do to keep growing and create that sustainable change. Yeah, but yeah, man, you inspire me so much. I can’t wait to– our elections are in 3 months.
Donna: You’ll somehow someway you’ll get there time will fly. Next thing you know, you’re graduating and you’re going to be a psychiatrist yourself.
30:32 Debunking Misconceptions of the Medical Field and School
James: One can only hope, yeah. But in that case, so, since we’re talking about the future, to some degree, I think you now being a PGY-1 at Stanford. That’s huge. I feel like something that we as medical students and we as, like, you know, not doctors yet, there are a lot of misconceptions we have about what’s to come, whether it’s even just about medical school or residency or about being a doctor 101, you know, one of the first personal huge misconceptions I had about medicine that I hear from my mentors, you know. It’s not all fun where it’s all treating patients all the time. Like, what I’ve been told is that there’s a lot of paperwork, like, more than you can possibly imagine, you know? And so, in that theme, what are some common misconceptions about the medical field or medical school in general that you think requires some clarification or something that you would like to enlighten our listeners on?
Donna: Ya, so I agree with what you said. And I’ll just kind of integrate and echo a bit of what I also said earlier. Like you said, I think the biggest misconception is that you go through all the schooling and, you know, we expect to come out and feel like, you know, Gray’s Anatomy is doctor. Right. Like that’s totally not how it works. Not even with that level of trauma. I like when I was in medical school, I really took that time for granted. Because it was really hard, right? Like you dig your nose into the books. And you’re like, okay, once I learn all this information, I spit it out, I take STEP1, STEP2, I go to residency, you know, I’ll just like magically know everything. And the whole system will make sense. Speaking as a PGY-1, that’s not the case, but probably physicians who are veterans even, you know with years of experience under their belt, they could probably still tell you that like the system still doesn’t make any sense even though you’ve been out of med school for so many years. And so I guess but you know misconceptions, the biggest misconception I had in medical school was that I thought going through medical school and graduating would give me this magic wand to feel better about myself and about my job and career in medicine. And that’s just not the case. So if you’re waiting to feel better magically at some point, sometime – it’s kind of parallel with adulting right? Like there’s no adulthood ceremony even though you know 18 is like the legal age and then 21 you can drink, right? You graduate undergrad. But there’s no like– you know, oh, at 25 now you’re magically an adult because you can actually rent a car. I think it’s like 24, 25 or something. And then at 26, you’re off your parents like insurer, health insurance right? There’s no magical ceremony that will graduate you into adulthood, that will graduate you into doctorhood and make you feel better at all. And so I think that that cognitive dissonance between your expectations and the reality of medicine in this world is very jarring. I think medical students and doctors live in our bubbles a lot of the time. And that’s why with like, you know, white ivory tower schools, you know staying in academia, like, there’s even a problem with physicians like talking to their patients, like half the time, like, we say these all these huge– jargon. And these patients are looking at you and they’re like ‘uh-huh’. Like we can’t even like communicate with our patients sometimes. And I think that’s a reflection on our own notions as a physician community. And in thinking that once I go through these like rites of passages, right, pre-med, med, you know, residency, attending, then life’s gonna be a hundred times better. And it just doesn’t. And so what I say is that, you know, during along this journey, you should just try to experience the journey for itself and find meaning for what you’re doing right now. If you’re always thinking about like the next step or having to achieve the next step, then I’ll be happy or then I’ll be successful, then you’re never going to feel fully whole and fully happy until you’re on your deathbed, right? And even then, people still have regrets right before they die. So I think being a doctor is a very cautious choice, like, about what you want to do and about the realities of it. And so, you know, I know it’s hard not to pigeonhole yourself into thinking about the next step, or about this perfect system that’ll magically appear to you on a red carpet once you graduate med school, but it’s not reality. If you look at data and research just in general, like that’s like, you know, physicians are twice, I think, yeah, two times at a higher risk for depression and mental health distress than the general population. And there’s a reason why, right? So yeah, I would say that’s the biggest shocker that I have learned throughout my years. I’m still learning now, right, and it’s hard for me to take my own advice. So hopefully, like, if someone out there is listening, than you can take a step back and just really reflect on your journey as you are showing up right now. There’s no other expectations for you than for you to just be yourself right now.
James: That is very wise, Donna. I think especially something that a lot of, for example, maybe our younger viewers or the listeners can relate to is that like, speaking on my own behalf, I remember I always looked at my parents and thought, wow, they really know, like, they have everything under control.
Donna: No, they don’t. No, absolutely not.
37:07 This Or That? Questions
James: Exactly. No, they don’t. You know, and I’m like, I remember thinking when I was 21, it’s like, oh maybe when I’m finally in med school or when I’m done with – I’ll feel like more under control, more grounded. But no, it’s literally just take everything one day at a time, you know? So thank you. Thank you for sharing that. That is definitely something that needed to be expanded upon. That is wow. Thank you, Donna. In any case, we’re coming to a close for this next episode of the APAMSA Podcast, and on a more lighthearted note to get to know you better on a more personal level with a couple of This-OR-That questions. So It’s simply an A or B, choose one, just let your heart decide.
Donna: Alright lets go.
James: Awesome. City or beach?
Donna: Beach, sorry guys.
James: Cats or dogs?
Donna: Dogs, I have one next to me.
James: Boba Princess? Princess Boba? Text or call?
Donna: Like what I prefer? Or– see I’m overthinking it. Text, I’m terrible, I’m a millennial, we just text we don’t want to call
James: Black or white?
Donna: Black
James: Morning or night?
Donna: Night owl
James: Summer or winter?
Donna: Summer, I was also born in July so, Summer forever.
James: Breakfast or dinner?
Donna: I’m a dinner girl.
James: Would you rather have the power to be invisible or the power to read minds.
Donna: As a psychiatrist, 100% read minds. Well I guess that would make my job too easy I wouldn’t even have to talk to the patient, I would just be like “I know what you’re thinking” and bam, bam bam. That’s it. But also if there’s a way to shut it off that would be nice. Like selectively using my powers.
James: Ya this is supposed to be a rapid fire segment but I do have but I do have to say I remember one of the things that um, psychiatry during my psychiatry didactic block, there was this like exercise that our professor had us do where we were all talking basically at like max volume, you know, and we were assigned to like, try to remember a list or something. And basically by the end of it, like we could not hear our own voice, our own thoughts based off like, over everybody else. And it was supposed to mimic like, you know, hallucinations or, you know, people who suffer from that. I was like, if you have the ability to read minds and experience what our patients are experiencing, that would be pretty wild, you know? But in any case, would you rather have a hundred thousand to spend on yourself or a million you can only spend on others?
Donna: Oh, a million to spend on others, cause then, I don’t know, I’ll just ask my mom to just buy me stuff. I don’t know. I’m joking.
James: And then we have two more. One of these is, I will only ask of you to cater specifically towards our special alumni guests. Indoor or outdoor climb?
Donna: Oh indoor. I’m sorry, I’m a weenie, I don’t know how to outdoor climb yet. I know, I wanna learn. It’s on my list to do.
James: If you ever find yourself back in Vegas I will take you to Red Rock.
Donna: That’s classic rite of passage right there.
James: Exactly. And then finally would you rather retake STEP1 or retake the MCAT?
Donna: Oh 100% STEP1 100%. So I, so I used to teach MCAT as well but MCAT just doesn’t it doesn’t make sense like the O-chem, the physics, I did not care about it. Also, I think MCAT is more miserable because you can retake it multiple times. Whereas for, I mean, there is a passing score-ish, but like with STEP1 you just need to take it and pass. So I’d rather do that versus MCAT, you have to retake it multiple times if you don’t, if you aren’t happy with your score. I feel like that just messes people up. ‘Cause how many times did you remember hearing your friends say, oh yeah, retake the MCAT again. That is like years of your life. I feel like that’s more hellish than just taking STEP one once and then passing it.
James: Absolutely. I have not taken step one yet, but I will eventually.
Donna: It’s pass or fail. You’re going to pass. You’re going to pass. Like, it’s going to happen. You’re only going to take it once and then you’re done. Whereas MCAT, it’s like, I’ve never used O-chem again, just FYI. I’m very starched, like advocate against O-chem. Just not using it. Yeah.
41:20 Advice for Pre-Health and Medical Students
James: Nice. Well, in that case, that brings us to the end of our This-or-That segment. Thank you for your candid and thoughtful responses. As we wrap up, we love to close out our one-on-one series by seeking advice from our incredible guests. I know you provided a lot of wisdom with our misconception question, but I would still like to ask anyways, if you have anything else that you would like to share, is there any piece of wisdom or advice you’d like to share with somebody navigating the journey of medical school slash medicine?
Donna: Absolutely. So I would have to confess that this is not my original thought, and I don’t even think it was this person’s original thought that said it, probably honestly came from Nike marketing. So I actually saw Mr. John Chu, who’s the director of Wicked and also Crazy Rich Asians up in SF. He’s doing a fireside chat talk with Aquafina. It was super awesome just seeing them like chatting on stage and talking about their lives and the creative arts of film. A really like great breather from medicine. And he was asked a lot of these questions as well and advice for people, etc. And I remember distinctly the moment, he was telling us that he was teaching a class at USC and he was sitting at I think some like loading dock or something. And he was crying because he wasted five years of his life trying to make another breakthrough film after Steven Spielberg had discovered him very early on at film school. And he felt like he was wasting his life and not moving forward. And the breaking point was him, was that he just realized at some point he said you just have to go do it. Just do it. That’s it. Three simple words, just do it. And it’s like three words that’s on like a Nike logo, but I was just listening to a story and I was just like know what he’s right like if I don’t do what I want to do now, what I’m passionate about, then one, no one else is going to do it, and two, or someone else is going to do it. And I’d rather do it because it’s something that I’m passionate about. And so I think that that advice really kicked me off to continue wanting to start up the National Asian Physician Association, NAPA, with APAMSA. So really thanks to, you know Mr. John Chu, who’s the director of really famous movies, just giving really good advice. And it didn’t even come from like a doctor. It came from a director, a film director, right? He was just like, just do it. And I was like, you know what, you’re right, Mr. John Chu, I’m gonna go do it. So, yep. I hopefully, like, if anyone’s listening out there again, like, if there’s something you just want to do, just, just do it. If there’s any doubt in your mind and it’s not obviously illegal or bad for anybody, like just start doing it. You be surprised how far you can go even if it’s just a little bit a day at a time. And it’s going to take a day at a time. Nothing’s going to come, success doesn’t come overnight. It just really, it takes 10 years for success to come overnight. I don’t know if people’ve heard that saying before, but that really speaks to volume about preparation, opportunities, and persistence in regards to success.
James: Wow. That is an amazing piece of advice. And definitely, it’s something that I needed to hear, especially about, from our earlier offline conversation. But in any case, Donna, Dr. Tran, it’s truly been a pleasure getting to know you better. We are so grateful for the time you took out of your day to join us and share your story, and even more so, all the time you dedicated to being a leader in APAMSA. To all of our listeners, we hope you enjoyed this episode as much as we did. Don’t forget to tune in next time for more inspiring stories and insights. Take care.
Episode 3 - A Conversation with Ashley Tam

Listen here:
YouTube
Spotify
Apple Podcasts
This episode was produced by James Chua and Ashley Tam, hosted by James Chua, and graphic by Callista Wu and Claire Sun.
Timestamps:
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
00:26 Introduction to Ashley Tam
03:28 Baking Cantonese Pastries and Buns
07:41 Playing Genshin Impact
11:26 The Journey to Medicine
14:31 Choosing Pathology as a Specialty
22:24 Clinical Skills in Pathology?
24:50 Why Did You Join APAMSA?
31:05 APAMSA Core Memory
33:21 2023 National Conference Theme
35:07 Wishes for APAMSA’s Future
37:18 Community Impact Week 2025
39:16 What Are You Looking Forward to in Your Medical Career?
41:46 This or That? Questions
45:14 Advice for Pre-Health and Medical Students
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
James: Welcome everyone to the third episode of the Asian Pacific American Medical Student Association Podcast, from roundtable discussions of current health topics to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization, this is White Coats and Rice. My name is James Chua, second year medical student at Touro University, Nevada, and the current Fundraising Director at APAMSA, and I’ll be your host for today.
00:26 Introduction to Ashley Tam
James: On today’s episode, we are thrilled to welcome Ashley Tam, an alumnus of Cornell University and current fourth-year medical student at Oregon Health and Science University. Hailing from Oregon, Ashley’s path to medicine is truly inspiring. As the daughter of Chinese immigrants, her upbringing was deeply influenced by the richness of Chinese culture and traditions. However, it wasn’t until her time at Cornell that she fully recognized the importance of her cultural identity and what it plays in her life. In 2020 she began her medical education at OHSU and by her second year, Ashley and her local APAMSA chapter hosted the National Conference at their school themed: Renewal: Out of the Flames, Into the Future. Ashley has worn many hats within APAMSA from National Conference Director to Co-Social Media Director, and now, Communications Vice President. Her dedication to the organization highlights her passion for amplifying AANHPI voices and fostering meaningful connections within the community. Beyond medicine, Ashley’s interests are as vibrant as her professional achievements. Whether exploring Teyvat and Genshin Impact where she boasts over 1300 days of active gameplay, watching anime, or being a proud dog mom to Goji, her spirited Shiba Inu, Ashley embraces life with enthusiasm. Without further ado, join us as we dive into Ashley’s journey, her unique perspectives on medicine, and the vibrant passions that shape her world. Ashley, welcome to the show. How are you doing today?
Ashley: I’m doing good. Thank you so much. That was a beautiful introduction. I love that.
James: Yeah, I said this in Vic’s as well, but a lot of the stuff is drawn from previous APAMSA bios, so if you don’t recognize that, then you know from I think 20–, year first National Conference.
Ashley: Yeah, that is triggering some memories for sure of like typing that up and submitting it.
James: Yeah, I remember for me, since this is my first year on the National Board, I had no idea what to write for my bio. And I think the example that was given was like, one, written in third person, two, it was very long, and so I was like, oh perfect, let me do something very similar. And then I took the time to read everybody else’s bios, and I was like, hmm, no one else took this approach.
Ashley: Yeah, I– like as Comms VP this year, I definitely go through, you know, everyone’s submissions when they submit their bios, because we need to get that prepared for our website and everything. And it’s really interesting to see the different approaches people have, like some people super, super long and some people like don’t include their hobbies and I reach out to them and I’m like ‘Hey, like what are some fun things you do outside of school?’ Um, so it’s fun to see people’s interpretations of you know, the prompt.
03:28 Baking Cantonese Pastries and Buns
James: Yeah, absolutely. And speaking of hobbies, one thing that I did want the listeners to learn about you personally is that I remember when we were talking about or like preparing for the podcast, one of the things you mentioned is that you are a baker.
Ashley: Oh yeah. I mean, I’m not like an expert or anything like that.
James: Well in that case what do you think is your favorite thing to bake?
Ashley: Hm. I think, similar to a lot of people, it’s like my baking journey kind of started around the height of COVID because I was like at home. I had a scribing job, but you know, at that time, they were like, you should probably not come in. And so I was at home, my family’s at home, my sister is doing school from home and I’m like I have nothing to do right now because I’m basically waiting for med school to start. and I decided to bake because I don’t like cooking as much because I’m more of a recipes person, and I feel like baking sort of like scratches that itch for me because it’s like a little bit more scientific. You really need to measure things out. And so because we weren’t going out to buy things as much, I decided to make egg tarts. And like I went through like a couple iterations. I mean, not my own recipe, this is other peoples’ recipes. But like the way that I did the recipe, I feel like I messed up a couple times and it didn’t turn out the way I wanted to, but then I really got into baking egg tarts during COVID. Then I pineapple buns as well, and then like the Cantonese cocktail buns which are the like still a milk bread bun but then the inside has like a coconut filling. So I made that sort of in rotation for my family. I’m like, oh, our stock is running low so I’m going to make some more. ‘Cause also I’m a little bit bored so I’m just like keeping up our stock and everyone gained weight over that time because I was baking so prolifically. But those are my favorite things to bake because I never thought that I would, you know, be able to make that at home. It’s always something that we have to go out to the Cantonese bakeries to buy. So it was really cool to be able to sort of provide that for my family at that time.
James: Absolutely. And I think like, for me personally, I’ve always also and I feel like this is applicable to many people in the science field how they prefer the science of baking to just cooking which I do both but I feel like cooking is a lot more about vibes than anything else. But yeah, when I was reading your description about like all the things you’ve made before, the three items you wanted to highlight. I actually last night and now that I’m finally on winter break. I finally have had the time to do the things that I’ve wanted to do. And one of those things on the top of my list, because when you’re a busy medical student, all you can really focus on is studying, right? One of the things on the top of my list was baking. And so the thing that I made most recently were Bolo Bao inspired. They were inspired cookies though. So it had like the topping of the bolo that makes it look like a pineapple. I guess. Or I…
Ashley: Yeah! Yeah, yeah. That’s awesome. Was it successful?
James: I’ll show you a picture and you can be the judge. Um, yeah, it, the base of the cookie was this like brown butter experience. So it was just like, it tasted just like a normal cookie. And so I’m like, now I’m actually right after this about to go to Dim Sum with friends. So I was gonna try like- gonna try like an actual pineapple bun and be like ‘how does actually compare?’
Ashley: Yeah. That’s awesome. You should, um when you go you should get the custard filled one. That’s always a fun one.
07:41 Playing Genshin Impact
James: Yeah, and so on a separate note though, something that I wanted to ask more about. So, over 1300 days of Genshin Impact. That’s, for the listeners, I think over four years if the math translates.
Ashley: It is, yeah.
James: How did that start?
Ashley: That’s a… that’s a great question. I think the launch of the game started, it was in like October 2020. I sort of had my eye on it, but you know, I was in my first year of medical school, I was doing didactics. And I was like, well, I don’t think I have time to like commit to starting a new game. I never played any like Gacha games before, but it just like really interested me. And then, it wasn’t until I think February when we finished one of our blocks we had just taken finals and we had a week off afterwards. And I was like oh, maybe I’m ready now, to like start this game and we’ll see how it goes. And you know, I think I started playing around February of 2021 and like the rest is history. Like, I’ve really liked it when I first started and because I had that week long break I was playing it like a lot and so I got really invested in it when I first started. And then, uh, Genshin is just one of those games where, you know, if you want to be free-to-play you kind of have to invest the time to be able to get the characters that you want and to be able to progress through the game easier, and so ya, because I really liked it I was okay investing that time. And it was like fun to you know, “I have to do dailies, I have to do my weeklies” and then it just becomes part of my list of things to do, not in a bad way. But it’s like, fun to keep up and to be able to feel like I can look forward to the next update and feel like prepared for like the new characters that are going to drop. Like I’ve come very far. And I’m proud of it to some extent. I haven’t spent money on it– my own money. I have had friends who have given me some like a birthday gift or like a Christmas gift. Like here’s like an Apple gift card and like I appreciate it but I haven’t spent my own money so I feel a little bit proud of that.
James: I feel that. Yeah. I used to play Genshin Impact and I also took pride in the fact that I was also a free-to-play player. But then like, eventually it got to the point where I did not get the 5– I lost my 50/50.
Ashley: Ugh, the worst. I think I have, on the poor side of luck with Gacha pulls. It’s like, a little bit upsetting sometimes. But it is how it is, so like I ration my Primos a lot. So I’m like, “I’m going to like hold out and like skip this character” because I know there’s another character that I will want later. I feel like I have relatively good Primo management. And yah. It’s a lot of I guess, self control.
11:26 The Journey to Medicine
James: Yeah. Absolutely. And see the reason why I want to bring up these hobbies and I do this with all of our guests. It’s to sort of show how like, medical students are not simply just, we’re not glued to our textbooks at all times. We are people, we do take care of ourselves in all shapes or forms, whether it’s like baking like you do, gaming like you do, or traveling, like whatever it is that keeps you grounded, you know. And so, I think I’m now very interested, I think our listeners would love to know, how has your journey been to medicine? Like, where did it begin? How did it get to OHSU? Like wherever you want to start personally.
Ashley: Ooh, I think my mom like pulled this out of the storage closet really recently but in first grade there’s like this art thing that our teacher had us do. And it’s like a picture of us and like ‘when I grow up I want to be’, and I had written doctor. So I guess like that’s when it started. Why did I wanna be a doctor at that time? I have no idea. I don’t know who put that idea my head. Is it because I grew up in like, an immigrant Chinese family and, you know, the classics careers that they love their kids to have, it’s like a doctor or lawyer. Something cool like that. I don’t know. But I think when I decided that I really wanted to pursue medicine was just through science classes and being really interested in the human body and like anatomy and like how everything functions about anatomy and physiology was super cool because you’re like wow it makes like total sense like how this works in the body and then it triggers this. And then it’s just like the science of it just makes so much sense, like the logic, and I thought that was really cool. So I think I decided at that time that I really wanted to pursue a career in the human sciences. Um, and I think I always sort of had an interest also in like the molecular side of things, like similarly how the logic of the human body is super cool. Like, I thought the logic and processes of like cells on a molecular level is also super cool. And so I think that’s sort of what, that was like the foundation for me finding interest in pathology because pathology is kind of like a specialty that is very granular and you have to look at like – you know number one it’s very small you’re literally looking under a microscope but there’s a lot of details that go on in pathology. And my love for that probably stems from my love for like details of molecular biology and stuff like that.
14:31 Choosing Pathology as a Specialty
James: Absolutely. And I actually, it’s interesting, because I would love to learn more about your journey to pathology because as far as I’m aware, you did, it was last year I think? The pathology fellowship, right?
Ashley: Yes, yes.
James: Yeah. So for me personally, like, I was actually very interested in pathology. There were only two specialties that I really, like, were leaning towards when I started medical school, leading up to medical school. One was psychiatry and then the other was pathology. And so…
Ashley: Super different!
James: Very, extremely different. And I think, like, my interest in pathology, stemmed from like, I did a post-bac, they taught it so well there. I also worked in so many research labs and I like that setting, right? Yeah. But then by the time I actually started medical school, I found that the way they approached pathology at my own personal institution made me like lose my spark for it.
Ashley: Oh no!
James: But, it’s fine! I was also in cadaver lab and I realized I didn’t want to do like forensic pathology.
Ashley: Yeah that’s fair.
James: Yeah but maybe you can re-inspire me so could you please tell me and also our viewers more about your junior pathology, post-junior pathology fellowship and how that really – I’m guessing it really affirmed like what you wanted to do.
Ashley: Yeah. I think I came to my decision of specialty a little easier than other students in general, not specifically like just in pathology, but I had exposure to pathology in undergrad actually because I did some shadowing. And like you I had been in some research labs before and I thought like bench work was really cool. And I was thinking, oh, I know what a research lab looks like, what that setting is, like the bench work but I don’t know what goes on in hospital lab and then so I did like some Google searching and I was like, oh pathology, that’s something that exists. And then there’s pathologists that like run the lab, whatever that means. And so I ended up shadowing some pathologists at a hospital that was close to my undergrad campus. And I thought what did was super cool. At that time when I was shadowing I basically sat at the scope with them and they walked me through how they were looking at cases and making diagnoses. Like “oh, this is what I’m seeing on the slide or under the scope”. And they’re showing me like what all the different cells were what all the architecture was, and it was hard to follow along because I didn’t have a lot of histology background, like at all. But I just thought it was cool how they could look at something and make a diagnosis off of it. And that you can actually see what disease looks like under the scope. And then they also use a lot of other tests like there are stains and stuff. And I just thought that, that logic puzzle was super cool because they’re like “okay so if you know this stain is positive and this stain is negative then I can say like it’s probably this diagnosis”. And I thought that was the coolest thing. And so I already had this. I was already like, inspired by pathology coming into med school. And so, you know, as a good med student, I tried to like, keep all the doors open and keep my mind open to everything that medicine had to offer. At my school I feel like when we had pathology lectures. When the pathologists came and gave us lectures, I was like super inspired by them because they were like super happy it seemed like they really liked what they were doing and they really liked the things that they were teaching. So that was a big plus. I mean, I already have like positive vibes about pathology but interacting with those pathologists I’m like “wow they’re super happy and super excited about what they do”. And eventually, I learned that there was this post-junior or sometimes post-sophomore pathology fellowship at OHSU. And there are, a handful of schools across the country that offer programs like this. But it’s like a completely optional thing, it’s not something you have to do if you want to pursue a pathology residency. There are plenty of people who don’t do that. And then, there are people who do a year in pathology but they go into other specialties. But it’s like, you know, maybe they have an interest in pathology, or they feel like they wanted to take more time to sort of think about what specialty they actually want to apply into and stuff like that. So people have a lot of reasons for doing it. I personally wanted to do it because I had heard from other people that it’s hard to get exposure to what the life of a pathologist is in med school because you know, it’s not a required rotation, there’s not that many elective rotations available to explore pathology and the fact that it’s just so different from the workflow of any of the other specialties. You can’t really get a sense of, a similar sense of what pathology is on a different rotation. So, and I was okay with adding another year, I know that can be a barrier, but I was like, you know what, I think I want to do this because I really want to know what pathology is all about. So I ended up doing that between my third and fourth year of school. And it was awesome because I– because it was between my third and fourth year of school, I had already finished all of my third year core rotations before starting. And so I had already gotten exposure to, you know, generally a lot of other specialties. And then that first month of orientation of my post-junior fellowship, I was like learning how to gross, I was learning how to use a microscope, learning how to write a report. And even in that first month when I wasn’t like really doing anything real. I was like sort of clumsily like trying to figure out like how to be a pathologist. That first month like sealed the deal for me. I was like, I’m definitely going to pathology. This is like so much more fun. I’m like coming away from those days so much more excited. I’m coming home like really wanting to tell my husband like what I did that day. And I felt so good about pathology, like all the other doors are for sure closed at this point. And then the rest of the year was just like super fun because I got to really just like learn what I wanted to do as like my future career. And I think the program was really cool because you essentially get to work like a PGY1 pathology resident. So you’re really integrated into the residents’ schedule, like you staff a service by yourself and sign out one-on-one with an attending. You’re not reporting to your other residents, you’re part of the team. And so it was, it was a really fun experience for sure. And it solidified my love for pathology and it also helped me learn so, so, so much.
22:24 Clinical Skills in Pathology?
James: Absolutely. I’m very interested to hear your thoughts, so one of the things that like, people really brought this up to me. And I feel like it also I feel like it applies to psych or psychiatry in that like, it’s sort of unfortunate that all of the clinical skills like the actual clinical skills like how to listen to heart sounds, it’s sort of like you don’t use it as much in pathology. So I’d love to know what are your thoughts on that?
Ashley: Of like learning clinical skills that I won’t use like as a pathologist?
James: Yeah!
Ashley: Um, I mean, I guess that’s just like the game of med school. Is like, doing a lot of things. or like learning a lot of things that you might not use but are important to explore all that medicine has to offer. I guess it’s just like, you know, a means to an end. So, I guess I never really thought about like “oh there’s all these things that I learned but then like I won’t use it. So I will probably lose the skill later on in life”. Um, but I feel like that’s just the nature of med school and like without having learned, you know, how to listen to heart sounds and stuff like, I wouldn’t have been able to get like that, that full experience of exploring other careers in medicine. So I think I’ll look at it with that perspective.
James: Yeah, no, so it still was all very useful. Yeah, it’s a very positive outlook, and something I need to remind myself of instead of just saying like, “Oh, it’s all being wasted”.
Ashley: Yeah, yeah. I would agree. I guess I never really thought about that too much. But you know, like when you, when you start clinical rotations, like, maybe there will be something else that like, inspires you. And then it’ll open a door that you didn’t think could be open. So.
James: Absolutely. Yeah, well, we’ll see. I’ll circle back with you in eight months or so.
Ashley: Yeah, I would love to hear.
24:50 Why did you join APAMSA?
James: Yeah, and so that– I see like pathology and we’ve talked about your medical school career and the academic portion. But now I want to talk about the extracurricular stuff, and more specifically APAMSA. Let’s start with the beginning. Why did you even join APAMSA in the first place?
Ashley: You kind of touched on that a little bit in my intro. But you know, I didn’t find an Asian community that I, you know, could share. Or like peers. I didn’t find peers that I could really share my heritage with and cultural like nuances with until I got to college and I think it’s because Portland is not a super diverse city. And I did have Asian friends but I think like, my Asian-ness is something I only really appreciated with my family. And I think I never sought out to share that Asian-ness with my friends at that point. But then when I got to Cornell, like even my parents were like, “there’s like so many Asians here”. And they were super surprised about that. And I didn’t know what to expect, moving all the way to the other side of the country. But I actually found like a really large community of just like Asians and like I was actually able to speak Cantonese with with friends for the first time, outside of my family. And so I thought that was really cool. And I think that sort of unlocked something within me I’m like wow this is something that I didn’t realize I was missing but I really really like it. And so I came back to Portland and when I started med school I was like, I want to have that community again. I want to be able to have that community here in Portland. And also I guess I didn’t really interact too much with the Chinese community or the Asian community in Portland, and I thought it would be cool to serve that population here as well. Because I wasn’t really in touch with the community. And so that’s the first season why I joined like the OHSU chapter of APAMSA was to really find that community again and be able to do something with medicine with them. And then that was really fun. I really liked that, being able to have that community to lean on and depend on. But also to connect with outside of school. And then in terms of joining national board, OHSU had won the bid host National Conference. And National Conference directors aren’t elected they’re sort of like selected from the host school. And then so I had this opportunity to participate. And I was super nervous. I was like, you want me to like help run a national conference? That sounds crazy because I’m not really an event planner. I obviously had never planned an event to this scale before and I had a lot of doubts and insecurities and a big lack of confidence but my friends who were other national conference directors. They were like, you know, you should participate in this I think like you’d be a good addition to the team. I was like, okay, we’ll see. And so I became the National Conference Communications Director. And I had so I had so much fun doing that. I didn’t realize that, you know, using my brain like creatively and being like bit artsy. I’m like not a great artist but I do like doing some art. And being able to do that with the National Conference for APAMSA was actually really really fun. And I’m so glad that I had people to support me and give me that confidence boost where I couldn’t give to myself. So I’m super grateful for them pushing me to like get into this role and then you know by the end of the year I was like I want to keep doing more, I want to keep working on the national board, I want to keep working like artistically and creatively. And so I ran for social media director after the National Conference was over. And then, so, I kind of stayed on. And so that was super cool. And I’m really grateful that I have the opportunity to have this position because it’s super fun and I get to work on APAMSA, which, you know, has like the mission and the values that we all want to, that we all like are really behind.
James: Yeah, absolutely. I can definitely relate to that. Because I think like when people ask me like, why are you so passionate about this organization? I always immediately connect it back to my personal statement. And talking about I want to serve the community I’m a part of. And I feel like there’s no other organization that really does it like APAMSA.
Ashley: Agree.
31:05 APAMSA Core Memory
James: You know, and so looking back with this very like illustrious career in APAMSA is there one memory since your graduating right? Is there one memory that you’re going to be looking back at very fondly, like wow I did that you know with the rest of the National Board or like with your own efforts or however you want to answer it.
Ashley: Yeah, one core memory that will definitely always stay with me is on National Conference day. It was during the lunch period slash poster session period. All of my National Conference co-directors, we took group pictures in front of our photo booth area. And then I was like – everyone is out and about at that time. Everyone was gathered in the big atrium in the building so like lunch was set up there, the poster session was there. That’s sort of all the events that were going on at that time and so everyone was mingling about. And we were at the photo booth that was set up along the wall. And we’re like taking pictures and then as we’re taking pictures you can just see like the whole scene like everyone gathering, having fun, eating, talking to people about their posters and stuff. And I was like wow I’m so proud of us. And so proud of what were were able to do and to see a year’s worth of work culminate in one day. And to see people enjoy themselves and we’re also enjoying ourselves, yes there’s a little bit of stress, but it was like I felt so much pride in that moment. And like, I was almost tearing up. I was like, I can’t we’re taking pictures but like I felt like the tears I kind of like coming up because I was like just so proud of like what everyone was able to do and like we then took pictures with our committee members and stuff and yeah, I just felt like immense pride in that moment. And also just like I couldn’t believe that I was able to participate in something like this and to help bring something like this to life.
James: That is a really touching story. Are you attending the National Conference? This upcoming one?
Ashley: Yes! I bought my tickets and everything.
33:21 2023 National Conference Theme
James: And so for our listeners, the next APAMSA National Conference will be hosted at Duke University School of Medicine in North Carolina from March 7 to 9. 2025. Yeah. Hope to see you guys there. But, I actually wanted to ask you one more question about your guys’s National Conference, and it was a little bit ago, but how did you choose your theme? Renewal: Out of the Flames, Into the Future.
Ashley: Oo, that’s an interesting question. I was not the brain behind it. I was sort of the Yes-Woman, I was like this sounds great! It was our National Conference Finance Director, Hannah Moon. She’s a resident now! But yeah, she, I think she came up with this idea. Her and our, actually I think she was the main one behind it. Yeah. And I was like, it sounds great. I love it. And you know, the, my like comms director brain was going and then I was like, oh, out of the flames, a phoenix would be a great logo design and so that’s sort of where I ran with that. But I was inspired by her for the theme and then that’s sort of where our national conference logo came from.
35:07 Wishes for APAMSA’s Future
James: Gotcha. Yeah. And so on the topic of, you know, out of the flames into the future, now that your time, we cannot thank you enough for your time in APAMSA, but is there something that now that you’re graduating, moving forward onto residency soon enough. Is there something that you hope for, for APAMSA? Something you hope we do for the organization, some sort of change that you want to see, something related to the future of APAMSA, is what I’m asking
Ashley: That’s a great question. I think just like the growth of our organization. Like I think APAMSA offers so much to its members and like there’s so much support that APAMSA can give chapters to create, or host events, participate in health fairs, community screenings, and things like that. And I think those are super valuable experiences. And I would just love to make that available to like a lot of other chapters and so then they can like serve their communities in that way. I feel like APAMSA does a lot to serve the communities that all our chapters are in. And so just like seeing like the growth of our organization to more like more pre-health chapters because like there’s so many opportunities for mentorship. So I would love to see that. And just the growth of our organization so then, you know, we can inspire more students across the country, and then it can also just like serve those communities as well. So I’m like super excited to see that. Yeah.
James: Absolutely. I personally can’t wait as well to see APAMSA keep growing. And I’m sure like all of the hard work we as a national board have done this year will keep the momentum going for next year and so forth.
37:18 Community Impact Week 2025
Ashley: I’m excited for the event that you’re – that you’ve taken a big part in putting together. Your week of service.
James: Oh yes so for listeners let me make sure I get the date right, but what Ashley was referring to is Community Impact Week which happens from Sunday January 26th to Saturday February 1st, 2025. What she’s referring to specifically is that I wanted to create an event that sort of celebrated Lunar New Year through service, through philanthropy, through, you know, being there for the community. And so we’re, we invited every single medical school that is affiliated with APAMSA to volunteer during that week, to sort of show our presence in all of the local communities. Yeah. And so we’re going to be posting more about that as the days roll by. I’m sure by the time this episode is actually posted, it’ll be right around the corner. So I’m sure listeners will have a lot to see but yeah I’m very excited about that too. And I think on the topic of growth, um, in the topic of like how many members there are of APAMSA, like, I think the reason why I thought an event like this should occur is because like, there are over 180 chapters across nine regions of the United States. And I just felt like, even though we are all individual local chapters. It would be a nice opportunity for us to all come together in solidarity to do something for our AANHPI community. I think this really encompasses – also the importance of like, serving, like, of Lunar New Year, you know? It’s not just about celebration, you know, let’s get that good karma going right away.
Ashley: Yeah, yeah.
39:16 What Are You Looking Forward to in Your Medical Career?
James: Yeah, I’m very excited about that, but we have about one more month so that’s a little bit in the future. But I wanna talk about something a lot more in the future. And so with you graduating in 2025 and residency being right around the corner, there’s so much to look forward to in your career. You’re going to be a doctor in like less than six months, which is kind of wild.
Ashley: Oh gosh, I know. That’s crazy. My grandma was just telling me yesterday. She was like I’m going to start calling you doctor, and I was like oh my god. This is crazy
James: What is something you’re especially looking forward to in your medical career? As a doctor i guess.
Ashley: Um, I guess I from like a medical student standpoint right now. Something I’m looking forward to. It’s just like getting in to my career, like graduating residency and coming out. Most pathologists, I think, will do a fellowship as well. Like 90 something percent of people do a pathology fellowship so after fellowship I’m excited to just be like a competent pathology with the knowledge to be able to sign out cases independently, to be confident. I mean we’re going to be lifelong learners right? But we’re going to come out of training feeling like we can do things for real and not have to run things by someone. And of course there’s always like, you will come across things that are difficult or that you don’t know and will ask your peers. But I’m excited to do the work, to do the work and serve the people and to have the confidence to do that. I’m just like excited to get to that point. We’ve just been learning for so long, training for so long, I want to be the real deal. So that’s what I’m excited for at this point.
James: Absolutely. And I’m, I know I speak, I can speak for all of APAMSA and all of your friends and colleagues. We are looking forward to you, for you and that very bright future ahead of you.
Ashley: Thank you.
41:46 This or That? Questions
James: Yeah, absolutely. And as we come to a close for the podcast. We have two more segments to go through. If you guys, if you took a listen to Vic’s podcast episode, we like to do a quick rapid fire of This or That questions just so we can get to know you a little bit better. Because we know you’re a gamer and you like anime and a baker. But this is just quirky questions, you know A or B, really fast. Are you ready?
Ashley: Yes
James: City or beach
Ashley: City
James: Cats or dogs
Ashley: Dogs
James: Text or call
Ashley: Text
James: Black or white
Ashley: Black
James: Morning or night
Ashley: Night
James: Summer or winter
Ashley: Winter. I feel like I’m a holidays kind of girl, so I feel like that’s when all the fun things happen for me.
James: Fair enough. Breakfast or dinner
Ashley: Dinner? I do like brunch but I feel like dinner options are greater.
James: Mm. Would you rather have the power to be invisible or the power to read minds?
Ashley: Be invisible.
James: Would you rather have $100,000 to spend on yourself or have $1,000,000 that you can spend on others?
Ashley: $1,000,000 to spend on others. There was like this quote I heard that was like “why do I need something” or, “why do I need to have something that I only need to use tomorrow when someone could have that if they could use it today?” So I feel like that’s really stuck with me.
James: And finally as we are all medical students, would you rather retake STEP1 or retake the MCAT?
Ashley: This is probably controversial but I think I would take STEP1? It’s a longer exam, there’s so much more material that goes on behind it, but like, I feel like in didactics I was able to keep up with board studying and anki through didactics to the point where when I got to STEP1 like after doing practice questions and stuff I went into it feeling pretty chill. And I remember going into the MCAT feeling not chill at all. So I already have the potential to be chill going into STEP1 so I feel like I have the ability to get back there if I needed to.
James: Yeah, absolutely. And I don’t think that’s that outlandish of an answer. Unfortunately, since we’ve only asked this of two people, you and Vic, Vic said that her medical school didn’t require her to take the MCAT. So…
Ashley: Beautiful.
James: Yeah. I will keep you posted as we keep asking more and more guests of the pod which one is the more popular exam.
Ashley: I’m excited to keep listening.
45:14 Piece of Advice for Students
James: Well, in that case, that wraps up our This or That segment. We appreciate your candid honesty. To end all of our one-on-one series for White Coats and Rice, I always like to end it seeking out advice. So Ashley, what is one piece of advice you would like to offer someone in their medical school journey, whether they’re pre-med or someone who’s right in the middle of their didactics or rotations? You know, what is one piece of advice?
Ashley: I would say my piece of advice is to allow yourself to invest in the things that make you happy and fill your cup. I feel like it’s super important if you have hobbies that you really enjoy to really take the time to enjoy those hobbies and do them. I feel like it’s really important to have that outlet and something outside of school and the daily grind. But then in terms of like school related extracurriculars, I think it’s important for people to– like it’s ok to invest more time into an extracurricular that you really like and not as much into something that doesn’t fill your cup as much, that doesn’t inspire you and excite you. Like for example if you really like mentoring and tutoring and you don’t like doing research as much, I feel like it’s okay to spend more time doing tutoring and mentoring. You don’t have to do that research if you don’t want to. I feel like it’s easy to fall into the trap as a student who is reaching for that next step, that next milestone, it’s easy to feel pressure to do everything under the sun to try to get yourself to that next point. And ya, just give yourself grace and allow yourself to do the things you like to do because there’s a lot of required things that we have to do in school, whether it’s– you know you have to do a didactics block or you have to do a core rotation and you’re not going to like everything. It’s impossible to like everything that you’re exposed to in medical school. If you do, then great but I feel like that’s not the case for most people. So because there are all these requirements and the schedule is really tough and you’re always working, I feel like it’s important when you do those extracurriculars to be doing something that still can inspire you and can keep your love for medicine alive and keep pushing you towards that next step. And it’s totally possible to build your CV and to do something you like at the same time have that overlap and be the same thing. I think that’s something that I’ve sort of worked on and I know– I’m sure other people feel the same way. So just know that, I think it’s ok to invest your time into something that you like to do.
James: That was sweet. In any case, thank you, Ashley. It has been such a pleasure getting to know you better. We hope that you keep your cup filled as the rigors of residency are around the corner. We’re so appreciate of you taking the time out of your day to share your story with all of us. To all our listeners we hope you enjoyed this episode as much as we did. Don’t forget to tune in next time and regardless of what time you’re listening to this episode, happy holidays and take care!
Episode 2 - Ask Me Anything with Dr. Caroline Park

Listen here:
YouTube
Spotify
Apple Podcasts
This episode was produced by Annie Nguyen, Reanna Dona-Termine, and Ashley Tam, hosted by Annie Nguyen, and graphic by Callista Wu and Claire Sun.
Chapters and Time Stamps:
0:00 Introduction to White Coats & Rice: An APAMSA Podcast
0:51 Introduction to Dr. Caroline Park
2:33 The Medical School Train and Fellowship Choices
5:46 Why Trauma Surgery?
7:30 A Day in the Life
9:47 Acute Care Surgery Lifestyle and Scope of Patient Care
12:23 Addressing the Mental and Emotional Stress of Surgical Specialties
15:37 Institutional Efforts to Address Mental Health
17:10 Representation in Surgical Subspecialties
18:38 Carefully Choosing Hobbies: Running, Gardening, Cats!
23:59 Living in Dallas
25:00 Moving to a New City
26:42 Choosing Where to Live and Finding Community
28:39 Managing Finances
31:16 Pursuing Research and Building Your Skillset
33:55 Advice for Those Interested in Surgical Specialties
36:35 Closing: What is One Thing that Brought You Joy Today?
0:00 Introduction to White Coats & Rice: An APAMSA Podcast
Annie: Welcome everyone to the 2nd episode of the Asian Pacific American Medical Student Association Podcast. From roundtable discussions of current health topics, to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization – this is White Coats and Rice. My name is Annie Nguyen, a postbac at Stanford University, and a member of the Leadership Committee at APAMSA. I’ll be your host for today!
This is our Ask Me Anything Series! Each month, we spotlight an extraordinary physician who shares their insights on medicine, life, and everything in between. This is your chance to ask questions, hear their stories, and learn from their incredible experiences. Whether you’re curious about their journey, their day-to-day, or their views on the future of medicine, nothing is off the table. Let’s dive in!
0:51 Introduction to Dr. Caroline Park
Annie: I wanted to first introduce, of course, our guest of honor, Doctor Caroline Park, who specializes in emergency general surgery, trauma and surgical critical care. Her medical career has spanned Boston, New York, Los Angeles and most recently, Dallas, Texas, as she has joined the UT southwestern faculty in 2018. Her research focuses on surgical critical care practices, outcomes in trauma patients, and integrating new technologies. And we’re very lucky to have Doctor Park here with us today. So let’s give her a little round of applause. And before we jump into some questions, Doctor Park, I just wanted to give you a chance to introduce yourself further and maybe describe your career, because it does seem like you’ve been, you know, all over the place.
Dr. Park: Yeah, I first of all, I want to say thank you to you guys. I really looked forward to this in our last sort of, interaction. It was wonderful. And I’m just so grateful to be able to do this. I’ve always wanted an opportunity to kind of give back to my community, and I never really quite figured out how to do it. So there you guys are. Just showed up. It was perfect. Perfect timing. Not really much else to add. I this is my first job, um, in Dallas and I’ve loved it. Um, I am a big city girl, and I think that might, you know, come up in some of the questions that maybe some of you guys have. So, uh, to not be afraid to, to kind of pick up and maybe move to another place because you’d be surprised by how much you learn. And, you know, these days it’s really not too it’s not too difficult to, you know, to meet your family and be connected. So, um, be brave.
2:33 The Medical School Train and Fellowship Choices
Annie: I really appreciate that. So could you describe more about what was the driving force between moving to Los Angeles? You were there for a short stint, I think, before the pandemic, and then now you’re in Texas. Was it the job specifically, like trauma surgery?
Dr. Park: Uh, yeah, actually. So, um, one thing that you’ll notice, and I think it sounds like a lot of students here are in medical school. Some of some of you guys might be, you know, applying to medical school. It is almost like a railroad. You kind of get onto the medical school train and it’s, a it’s kind of just goes in one direction. So honestly, the hardest obstacle, the most difficult obstacle, in my opinion, is getting into medical school. There is so much that you have to do these days anyway, right? So observer ships, clinical hours, research all those things in order to make it. And it’s very, very competitive. But once you’re on that train, you know, whether it’s good or bad, you know, you have preferences for where you want to go and it, you know, your fate is to some degree, sort of determined by an algorithm, like a computer, right? Like just how it was for medical school. So it’s kind of the same thing, with fellowship, which is advanced training. So, for example, you know, anyone who wants to go into surgery has to do a surgery residency, right? A general surgery residency. Um, if you want to go into orthopedic surgery, you have to do a residency in orthopedic surgery. However, if you want to go beyond being a general surgeon, which is still a really great job. You would have to do a fellowship. Now that’s more advanced training. That could be anywhere between 1 and 3 years, potentially. And, you know, it could be anywhere from pediatric surgery to surgical oncology to what I do, which is acute care surgery, trauma, critical care. Um, so at that point, you actually have a choice in where you want to be, because these programs now will become a little bit more diverse. So medical school, you have to take the same classes – anatomy, biochemistry, you know, all that stuff. Um, but when it comes to fellowship, there are what I describe as certain flavors. So maybe there’s a fellowship where you want to learn more critical care, or one where you want to operate on really big hernias, and you start to see those differences in those fellowships. So you kind of get a sense of what you want when you’re in residency. Like, I really want to focus on this, so I’m going to look for that place. You have a little bit more control. I guess what I’m trying to say is you get a little bit more control as you’re on that, you know, sort of that train and you can kind of figure out what your destination is going to be. And so that’s what led to me in Los Angeles was I was willing to come out of my bubble. I’ve been, you know, I was born and raised in the Northeast. I’ve survived multiple storms. I was getting tired of the weather. I, I didn’t like the fact that it was always dark when I woke up, and it was dark when I went to bed. Um, and I wanted to just try something different. And I was, I think that was the best decision I ever made. I met a completely different group of people, like, they do things differently, and I had so much fun. So, um, and it’s only a couple of years of your life. You’re not committed to staying out there. So I would highly recommend that you guys kind of go outside your bubble and explore. That way you can look back and say, you know what, I tried everything and I don’t regret it.
5:46 Why trauma surgery?
Annie: For sure. And you’re right, Boston storms are absolutely no joke. So I’m glad that you got some sunshine in LA. In terms of what was, you know, directing your freight train, if we want to call it that. Um, what drew you to trauma surgery or just surgery in general?
Dr. Park: I am very biased because I believe that surgery is the best, because not only do you get to diagnose something, you can treat it either minimally with medications or medical management to like maximum management. Right? So like with a scalpel, I, you know, there’s not a lot of people that can do that. And I think that’s why general surgery is even better, because, I mean, we truly take care of the whole patient. I mean, outside of like, you know, the head and doing bony, you know, bony injuries and things like that. I mean, you know, my scope of practice can be anywhere between taking, you know, an inflamed appendix out of someone to, um, you know, sewing a heart closed after, um, you know, someone got stabbed or shot in the heart to, you know, unfortunately, patients with, you know, really bad, peripheral arterial disease and had diabetic ulcers, and now it’s grown to infection in the amputation. I mean, it’s really wide. Um, and I’m very glad that, you know, we get such rigorous training in residency. The reason why it is five years long is because you have to know your anatomy. And not only that, you have to understand the disease processes. You have to understand, you know, what are the best options for this patient. Right. And then of course, like the last point is like doing the operation, right. The technical part. So I feel so grateful that we can constantly move from, you know, making sure we master all the concepts and the anatomy to like doing the operation and then managing everything else afterwards.
7:30 A Day in the Life
Annie: I think that there is an aspect of diversity here that you’re highlighting, especially in general surgery. And for someone who’s considering specialties that could be overwhelming to them. So to kind of clue them in, could you describe a typical day in your life?
Dr. Park: Absolutely. So, um, let’s say I’ll describe a call day… Okay. So I wake up, um, around six in the morning, which I know sounds very late to you guys because you guys are probably waking up much earlier to go to the hospital and see your patients and pre-ground. Um, but I, I go to I go to work, we do our morning sign out because sign out is very important. We have to talk about all the patients that came in from last night, all the ones that need an operation, you know, other people that are very sick that we need to know about. And we kind of prioritize, you know, what we’re going to do for the day. So for people who love a lot of control and want to know exactly what they’re going to do a few days prior, what I do is probably not the best for them because I literally roll into work and that’s that’s what’s on the list. Um, so but that being said, there are more common things that we do as general surgeons in acute care surgery, and that’s a lot of it is appendicitis, hernias, um, cholecystitis for sure. Um, and some other things, like they’re patients in the ICU intensive care unit who need tracheostomies, feeding tubes, biopsies. I mean, there’s so many things that I could be doing. So between really seven in the morning and seven the next day, I am in the hospital. Um, we get called about patients in the emergency room who might need a surgical, you know, they have a, you know, potential surgical problem. Um, I’m operating. So in between cases, I’m seeing these patients in between cases, um, I’m rounding on patients who are already admitted. And then that, you know, that happens pretty much throughout the whole night. And, um, thankfully, our cases are not very long. Now, some of you may already be in clerkships where you’re operating and standing for long periods of time. Um, I have to say that our cases are not as long as some of the other specialties, like, you know, vascular surgery or surgical oncology, where you’re maybe standing for like six, seven hours or time. Our cases are pretty short, mostly 1 to 3 hours. So I like that. I like the speed. I like being able to move between cases and patients. I prefer more volume of, uh, patients and taking care of them versus like the, you know, the length of the case.
9:47 Acute Care Surgery Lifestyle and Scope of Patient Care
Annie: You mentioned, before the call started, that this is just an interesting week because you’re actually in the ICU. So what is that?
Dr. Park: Yeah, absolutely. So, um, so let’s say I’ve recovered from that 24 hour call. I get to go home. Um, I don’t have to go. I do not have to go to work the next day. And, uh, I only take maybe, like, four of those calls a month, so I don’t want people to think like, oh, my gosh, there’s no way I can stay up for that long. You know, every other day. That’s not my life, okay? And I think a lot of people kind of get scared, or intimidated by, by that kind of lifestyle. But it is very, very doable. You just need to kind of pace yourself and, give yourself a break and let yourself recover. So the other sphere of acute care surgery, so there’s three in my mind. There’s emergency general surgery, which is what I basically just described. And then there’s trauma, which is, you know, trauma patients, trauma surgery. And then there’s critical care surgery, which is kind of in the middle. And there’s some people that like to gravitate towards one versus the other. And there are some people that are like a perfect Venn diagram, and they’d like to be just in the middle. And there are other people that really like more of the trauma. I would say I love all of that stuff. I can’t say I prefer more than another. I really do love taking care of trauma patients, but, you know, I love every aspect of it. Surgery is very, unique in that you’re going back to, like, medical school and you are looking at the patient holistically again. You are literally looking at that from head to toe. The neuro-, you know, the neurologic system, the cardiovascular system, pulmonology, GI, you, you know, infectious I mean, literally, we’re looking at every single system and making sure that we are addressing it. If there is an issue, there’s an infection, we’re treating it well, things like that. And I love that part, because it brings me back to all the things that some of you probably wish that you don’t ever have to remember, you know? Um, like things like the coagulation cascade. Right? You’d be surprised. There are certain things you actually do need to remember. The Krebs cycle hasn’t really been very applicable for me, but there are definitely things that, you know, there’s a reason why you learn all these things in medical school, so I love it. And the one thing that people sort of have some I wouldn’t say critical of acute care surgery, but they’re like, you know, you never really get to establish a relationship with the patient. You guys operate and they’re gone the next day. I would say that’s not really the case. I think in the ICU you could, you know, stay with the patient the whole week. That’s enough for me to feel like I have established a relationship with the family, to have rapport, for them to remember me in clinic, that’s good enough for me. I think some people wish for more. I think that’s that’s totally fine.
12:23 Addressing the Mental and Emotional Stress of Surgical Specialties
Annie: That was an incredibly insightful answer, and I think that you provided some really helpful metrics for anyone who might be considering this specialty in particular, such as, you know, preference on hours or volume. One thing is the emotional, and kind of psychological burden that comes with surgery. I think that’s maybe one reason why students will tend to hesitate. Can you describe what that experience has been like for you and how you personally address that?
Dr. Park: I think the biggest thing, and this is not unique to surgery, is being able to talk about things. It’s probably and, you know, I don’t want to make too many stereotypes about being an Asian American, but it’s not a strength that I had growing up was to talk about things. especially with, you know, with my parents, it was all about like, all the good things that you do are positively reinforced and then all the things that you don’t do well or, you know, you would never do that again. or even if you did do well, it was like, well, we kind of expected that. So, you know, like you got an A minus. Why why didn’t you get an A instead of an A-minus? You have to be willing to check your ego and realize that you’re human, and all of that sorrow and stress and tragedy is going to affect you at some point. And if it doesn’t, then I don’t know what to say. If it does, you’re human and it’s totally natural. And I would only expect that. And I hope that you are all surrounded by people who are willing to, like, debrief. Like, for example, if a patient comes in and unfortunately, this happens more often than we want, who comes in, you know, bleeding to death or has been shot. And we’re trying to do our best, but ultimately we can’t save that patient. It is a very hard thing for the medical students to witness, and I try to prepare them in advance. But you can only prepare someone so much. When they go through all that and they see kind of like really, truly how like, I don’t want to say violent, but it’s very it’s very involved. It’s very graphic. Right? It’s real. you can’t just ignore that and just say, okay, well, let’s move on to the next patient. You have to really talk about it. And I think it’s really important. Sometimes you’re busy and you just don’t have the time right now. But I would say if you feel empowered, you should feel empowered. And I hope that the people around you, your residents, your fellows, your staff, you say, you know what, we need to talk about this. So let’s just find some time and talk about this and just open it up and just see what people say. That’s what I would suggest, because at any point in your careers, all of you going into medical school, you will have to deal with death at some point. You will have to deal with something really tragic, and it’s going to affect you in a way that you did not predict. Maybe you won’t be able to sleep at night. Maybe you’re like, running longer and you’re just like, oh my gosh, I didn’t realize running for a whole hour. That happened to me the other day. I guess something was on my mind because I was running for a whole hour. I didn’t realize I’d run like seven miles. I’m like, gosh, I guess something is on my mind. So we all have different ways of kind of coping with that, so find some way to talk about it and some way to, in a healthy way, in some way to cope with it, and also in a healthy way.
15:37 Institutional Efforts to Address Mental Health
Annie: Embracing those really intense, visceral emotions instead of showing them down and pretending like they’re not there. As someone who has moved up in leadership and had various leadership roles, such as a medical director and now an associate professor, have you seen a more positive trend towards having those kinds of conversations, or have you seen institutions, make more of an effort to create those safer spaces for those conversations to be held? Or what work do you feel like needs to be done there?
Dr. Park: Yeah, absolutely. I think a lot of institutions are heading towards that. If they’re not doing it already, some specialties may, you know, should be doing better than others for sure. I would say that it has to come from your leadership. Because if your leaders are not willing to be open and receive that kind of feedback or have those kinds of open conversations, it’s not going to sort of percolate down, right? All the layers. So it does have to come from the top. And it has to be sincere too, right? Not just like, oh, just drop by my office whenever. Like, no, you have to, you have to be proactive. You reach out to people, you ask them how they’re doing. Right? And it’s not just like, hey, are you doing okay? It’s like, hey, like, you know, how’s your dog doing? Like, I know there was a bad storm and they get really affected by that, like those small things like that, that really that makes a big difference to people. It’s hard because we’re doing, we’re doing the best we can to take care of patients, and that is enough to do. It’s like super exhausting. You’re trying to take care of yourself, and now you’re trying to take care of your coworkers. Like it’s a lot every day, and you sometimes like your best every day. There’s this like, um, it’s not really a mem, but it’s like your best every day is so different. Sometimes it’s like down here and sometimes it’s way up there. That’s the best that you can ask from yourself.
17:10 Representation in Surgical Subspecialties
Annie: For sure. one thing that, just for the sake of transparency and for, everyone on the call who’s maybe trying to figure out a specialty, where do you feel that surgery falls in that spectrum of this willingness to discuss these things? If you have to be brutally-
Dr. Park: I, I’m maybe, I’m just like very, very lucky. But I feel like I’m in an environment where is very transparent and I feel very comfortable. maybe there’s some cultural differences, right? maybe in certain parts of the country, maybe in certain parts of the world. I mean, I hate to say it, but there are definitely some parts of the world where, there’s definitely more male surgeons than women surgeons. There’s not equal representation of, you know, underrepresented minorities. And there has to be a really good, deliberate effort to maintain diversity with excellence. It is not impossible. Um, people are too comfortable with, like, the status quo. And it doesn’t have to be like that. The status quo can be boring, and sometimes it’s not good. it’s not helpful for the people working the patients. All I can say is, when you guys are looking for programs, I mean, obviously most of you are already in medical school, but when you’re looking at residencies and fellowships and it’s something that you really care about, like representation, um, you know, look at the classes, what do they look like? It’s very easy to look at the residencies to see how well represented they are. Where are they coming from? Are they just coming from the same school that they’re associated with? That’s probably not a good sign. right. You want to get people who are from all over the place that are going to bring in new ideas. That’s how you learn.
18:38 Carefully Choosing Hobbies: Running, Gardening, Cats!
Annie: So we’ve touched on some interesting topics of finding community, dealing with difficult things head on. Um, and that is typically done best in community. But there are things that we can do for ourselves to stay grounded. And you had mentioned running as something that is one of your hobbies. I believe you’ve run marathons before. Um, plural, actually, which is insane. Um, can you tell us a little bit more about what you personally like to do to decompress? And maybe we had some specific questions about marathon training, but we can get to that too.
Dr. Park: Yeah, absolutely. You know, I think that, um, first of all, I never, I actually hated to I hated running when I was smaller when I was a child, and some of you guys don’t. This probably doesn’t even happen anymore. But there was something called the President Fitness Challenge in gym. So yeah, you’re looking at me like this never happened. So you had to, like, do this thing where you had to shuttle between two things. You had to, like stretch, you had to do a pull up. And the only thing I could do was stretch. I was terrible at everything else. I can never do a pull up. I still can’t do a pull up. But it wasn’t until maybe college, or maybe even after college when I was, I actually ran my first 5K. It was for breast cancer awareness and I was hooked after that. And I think I was hooked because it was a time where I was totally not distracted. I didn’t have my cell phone on me. I could just go out and it was my time and I could just focus on me. And that is not easy to find anymore. I know right now you guys probably feel like you have a lot of time, but there will be a time where you have 30 minutes to an hour and you have to be very, very deliberate about what you’re going to do. How are you going to spend that hour? You’re going to spend it on yourself. You spend it on someone else. You can spend something that you like to do or something because you feel like you have to do something else for somebody. So whatever it is, It has to bring you joy. What if in the past you had 20 hobbies, you may only have time for two? So, you know, just pick those things very, very wisely. For me, it’s like the running is easy. I don’t have to go to a gym. I just put on my AirPods, I go outside, I run, I come back, it’s very easy for me to do. Um, so long story short, I never, it was not something I love to do before, it’s something I like to do now. You can always start later in your life. my first marathon actually was in Los Angeles, and I finished it. The good and bad story of that race is that I wanted to run a 5K, but that was not available that weekend. And so I did the marathon thinking, well, if I don’t finish it, at least I tried. And so I finished it and that was awesome. So I don’t think I would ever do that again. Um, I’m not a big marathoner. Like the length is too long for me because I frankly, I just get bored. But, uh, half marathons are a great, great distance.
Annie: Okay. That’s insane. Did you train or you were just you intended to do the 5K, but then you just busted out 26 miles.
Dr. Park: I think I might have run up to nine miles before that, but I never. And this is the thing, like, you would think that as someone who’s like, used to like surgery, training and all the things that build up to being a surgeon, like you would think that I would have a good plan with running. But no, I just, I made up my own plan and it turned out fine, I guess, but I would not advise that. I would advise that you actually adhere to a running plan
Annie: That is deeply impressive. Um, I actually ran a marathon in April, and it was one of the hardest things I had ever done, and that required so much training. And so what.
Dr. Park: But have you ever done, have you done something that was equal, that was less hard and you were like, that was a breeze. Like this was nothing? So hard things put other things in perspective and I do think that that’s why some people push themselves so hard. They do these crazy things, the Spartan races, these marathons, because they’re trying to push themselves to the point where, like, okay, now any other obstacle that comes my way is like, okay, I can do this. I’ve done worse. I’ve been through worse before.
Annie: I actually haven’t realized that until this conversation, but that’s actually been my, the metric in my brain. Like, it can’t be worse than the Big Star marathon. Like it does not – oh, I love this. Okay, so any other hobbies, anything that brings you joy? You said normally it will, you know, whittle down to naturally like 1 or 2 hobbies. Is there anything else that you enjoy outside of running?
Dr. Park: I love gardening. I love like being outside gardening. I have lots of indoor plants. I have lots of outdoor plants. I think I like it because you’re watching something grow from a seed and you can see the direct effects again with surgery, like the immediate effects of if you abandon something, you don’t care of it, care for it, versus actually nurturing something, you know, paying attention to things, picking all the dead leaves off. I mean, all these things, I think, again, no distractions away from work, unrelated, focusing on myself. I think these are all things, whatever it can be for you guys. Right. Um, that can be your, your garden or something that you work on. Oh, I have tons of cats. And for a while during the pandemic, I was trapping, neutering, releasing cats, um, that were just in our community. I have never been a cat person. I’ve always had dogs growing up, and they just there’s this thing called the ‘cat distribution system’. I don’t know if you’ve heard of it, but they just come into your life. And so that’s what happened to us. And we’re like, we’re like, we have to save these cats. And so sequentially, we all got them, you know, neutered or spayed and released them back. And that was my hobby for a couple of years.
23:59 Living in Dallas
Annie: So all of these things that you’ve discovered in Dallas. So gardening, the cat distribution system, choosing you multiple times. what is it like living in Dallas? Is it easy to grow plants? Is the the cat distribution system more tame now?
Dr. Park: I think I feel like I have, um, affected the colony and at least in our neighborhood. So that that’s a good thing. I think I’ve impacted the ecosystem here because of that. I mean, it’s hot, like, I don’t I’m not gonna lie. Like, come from the northeast. It’s hot. But, you know, you just adjust. You just wake up earlier, you go running in the morning, you go running at night, you can grow things. And that the whole caveat here is like, grow things that are indigenous to this area. Right. Like and that’s the other thing I learned like don’t expect to be able to, you know, plant hydrangeas in the middle of the summer and expect them to survive. They’re just not used to that. And, you know, I’ve learned so much about the acidity of the soil and like all these things that I never learned. But that’s how you learn, right? You make mistakes. You make mistakes by planting something to late in the summer. It’s too hot. Um, so yes, I have tomatoes that I’ve grown, um, I have grown like my mom’s favorite flowers. Herbs lately.
25:00 Moving to a New City
Annie: I’m seeing consistent openness to trying new things. It seems like there is no problem with you trying something new, no matter what stage you are in your life. and that definitely seems to have helped you with all these different moves. Is there a ritual or like something that you like to do when you get to a new city? Um, especially for, you know, people who are going through transitions right now, what makes it easier to really immerse yourself in a new place?
Dr. Park: Yeah. This is not going to surprise you at all, but the first thing I do when I’m in a new city is I go running. I literally just I go running, I find the nearest river park, whatever, and I just explore. I think it’s a great way to see the city. You get to see all the sights you’re exercising. Um, so I would highly recommend that. So if you guys are ever going to conferences, um, I would say map out the city. You know, obviously you want to map out a safe route. Um, make sure, because I’ve almost done this before, but like, you run too far out and then you got to run back the whole distance, so you don’t want to make that mistake. Um, you know, and do your research, like, you know, if it’s like Chicago, right? Like, you know, go out to the lake, um, you know, do you want to get that slice of deep dish pizza that everyone, you know, talks about somewhere? So I kind of like to make a little, um, you know, customized itinerary, I guess. That’s another thing I like to do is, when I go traveling, and so I’ll map out a route and say, okay, I’m going to go here. I’m going to, you know, sample this, go to this coffee place, all these kinds of things so you can make it fun and sometimes around conferences or is a little bit of downtime. So I would recommend that you guys do that because it, it can be sometimes a little like, overwhelming to be in a giant conference with tons of people and just be in, you know, in a suit all day in an air conditioned environment, like go outside, get some fresh air, explore.
26:42 Choosing Where to Live and Finding Community
Annie: Perfect. And on that note, we actually have a question in the chat from Stephanie
Stephanie: Have you found it difficult to build community within each city that you’ve moved to? And then how have you, like, navigated trying to find community?
Dr. Park: That’s a really great question. I feel like I have thankfully been able to kind of choose the, like my most recent cities, so that I’m not in a situation where I really feel isolated. Now, I’ll put that in context. I’m a big city person. and when I was looking for a job, one of my specifications was I had to be in a big city. I know it sounds really silly, but as soon as I started to narrow down my job search, I started to look at how many Korean restaurants and H-Marts that were. Is it very important to me that I have access to kimchi once in a month. And I can’t explain why it’s so important to me, but it just is. Um, it’s important for me to have access to that. And one job just it checked all the boxes off. It was wonderful. The people were great. The mentorship was going to be amazing. I was going to have some great opportunities. There just wasn’t diversity there. And to me, it was not worth it. I felt that I could build those things and find those opportunities and be in a city where I would feel more represented, I guess. But, in a place like Dallas, like, I think it is relatively easy to find those pockets, right? So whether it’s like, you know, your culture, your food, your religion, um, you may have to try a little bit harder if you’re in a smaller place, but I’d say, like if you’re really committed and like things are really important to you and you’re looking at residencies or fellowships or even jobs you have, I make a list. I’m a big Excel geek. I look at my top three things that are non-negotiable things. Big city. Right. Diversity, and whatever my top third one was. Right. And if that if the program didn’t meet it, then I had to rank it lower.
28:39 Managing Finances
Annie: One other thing that has come up, for our students in navigating these transition periods, is just finances. And so people will range from having a lot of student loans to maybe not at all. do you have any financial tips that you would offer to medical students and residents, especially ones who might be trying to figure out their next big step?
Dr. Park: One of the things that really, um, used to bother me was when people are like, just don’t have your latte in the morning, just stop eating avocado toast, right? If those things bring you joy and it makes you more productive as a student, as a resident. Then, no, you get the latte and you get the avocado toast, right. There are certain areas where you can be more frugal, and there are other areas where you feel like there is more benefit. So for example, if it’s like, you know, sitting in a coffee shop every day and spending $10 on something so that you can really, truly study well and, you know, get through all your slides and do your work, then I’d say, yes, that’s that’s a great investment. But if you are, if you have multiple subscriptions to services and, you never use your Netflix or whatever it is, then maybe you need to start kind of looking at that, like, really take a look at your balance and see, like, do I use ClassPass or do I go to this gym? It’s kind of like purging your closet. You kind of have to take a good look at like what you don’t need and just let it go. Obviously that’s not going to take care of loans. But I would say about loans is, you know, thankfully now at least, I believe a lot of people got some of their loans forgiven, which, was which was great. Um, I still believe in the in the philosophy of living. Um, was it living like a pauper or something like that? Like even when you’re something, whatever, whatever the expression is, even if you have more income as a resident, as a fellow, even as an attending, I would still live frugally. everyone’s, uh, motivation is it’s like, okay, I’m a big, I’m an attending and I’m going to make my I’m going to make a, you know, a big purchase. And I want it to be a nice car or something like that. If it brings you joy, I think that’s great. But just again, be very mindful about like, you know what that means. And budgeting, it’s like budgeting is so boring and so tedious, but is actually really important. So for me it’s like, I don’t like grocery shopping. It’s something I really don’t enjoy. I don’t like going to the supermarket and smelling the peppers and the watermelons and enjoying that experience. It’s not something I like to do. I pay for a delivery service. It’s worth it for me. Just pick, think about the things that make you really happy. If it’s like the Pilates membership that you have and like it makes you feel amazing, it makes you feel energized or productive at work. It’s something you look forward to doing. You should absolutely spend money on that.
31:16 Pursuing Research and Building Your Skillset
Annie: It sounds like it comes down largely to really knowing yourself and making decisions based off of that. I see that Amber, you have your camera on. Did you want to ask a question?
Amber: I do, it’s kind of taking a turn from what you just discussed. a little more technical related to research especially now that medical school applicants and residency applicants have had more and more research each year as it goes by. Do you have any advice for either students who are applying or current students who are interested in either developing the research further, or even just being able to balance it along with our other commitments that we have going on?
Dr. Park: I’m not going to say I feel bad for you guys, but it is. Like I said, it’s getting so much harder. I don’t think I would even know what to do with the research project. I mean, yes, did I try to do some things? Absolutely. But I have some mixed feelings about this sort of expectation because you’re doing something just to kind of check a box off to say, yes, I did research. If you’re actually doing research to learn skills about, like, you know, basic statistics or how to do a systematic review, then fine. But to do research, like you really have to have like a decent amount of training and exposure to it. And I think it’s really unreasonable to ask, medical students who have had zero training to be able to do something. Now, that’s where having a really good mentor helps, because if you have a mentor who understands what you know what to do and can give you a reasonable project that you can, you know, either jump onto or help with, I think it’s great. But when you are tagged with a mentor who is not doing that and kind of abandons you and it’s like, okay, you figure it out, that’s where it gets really challenging. So picking your mentor is really important. And I tell medical students this all the time because they reach out to me for, for projects. And sometimes I don’t have anything active where I could have them as a lead. But you want to go in with this is what I know how to do – I know how to extract data from my medical chart. That’s a very useful skill that actually takes time to teach someone how to do it. Right. So if you can already do that, you’re really going to be like up higher than a lot of other students if you know how to organize data into tables, even better. If you know how to read an abstract, you’re getting up the ladder, right? So you kind of see how it takes like several, you know takes several steps to kind of build yourself up. So being able to say like, yes, I want to do research. Fine. That’s great. We love working with eager medical students, but I also need to know what you are capable of doing, because I don’t want to tag you onto something that you’re not gonna be able to do. You’re going to be disappointed because you’re not going to be able to get the project done on time. And then I’m going to be like, I feel bad because I wasn’t able to, give you the mentorship that you needed. So it’s two way street.
33:55 Advice for Those Interested in Surgical Specialties
Annie: On the note of, making yourself a more competitive applicant. Research is one huge thing. And thanks, Amber, for that question. Do you have any advice for students specifically who are interested in surgery? Any concrete advice, technical advice or just what you wish you would have known when you were going through the process yourself?
Dr. Park: Surgery residency, not research, right?
Annie: Yeah.
Dr. Park: Okay. Gosh, my path is so atypical. And maybe that will give some of you guys some hope who had very atypical paths, but I, actually didn’t want to be a doctor. I wanted to, like, work for the CIA. And my parents were not thrilled with that idea. I then tried to pivot and, you know, be in the health policy area because it was kind of similar. Not really. So I did my master’s in public health. I did that for a few years, and I worked for the city in New York City, the Department of Health. Um, and then, you know, I didn’t know I wanted to do surgery. So I got into medical school. I really I was, I was very I was an open book. I really, truly enjoyed everything. And not to say that that was a detriment, but it made it harder for me to decide what I wanted to do. And what I will say is your mentors and your experience and your rotations can change your life. You can have one bad month on a rotation that you thought you were going to love, and it’s going to change. You’re going to change your, your career. Like, oh gosh, I thought I wanted to do this, but now I’m, I don’t. And now you’re thinking, well, what am I going to do now? So kind of thinking about it, like, did I not enjoy this rotation because I just didn’t get well, the people and the culture or whatever? Or is it just like the medicine itself? That’s just not for me, right? So really kind of go into those rotations like, like thinking I want to be an expert in, you know, internal medicine. I want to be an expert in surgery. Like what is the life? Immerse yourself into that and think like, do I like this? Is this what makes me really happy? Right? Like I’m really tired, but am I still really happy? I’m not even thinking about it and it’s like, oh my gosh, it’s already 4:00 in the afternoon. Like the time just flew by. That’s how you know that you really like something. Um, and that’s how I knew that I like surgery because I would wake up at ridiculous hours. And I loved running around the hospital, and I loved helping the interns, and I just, I went home so excited to be able to tell my boyfriend now husband like what I did that day, right? And so, like that excitement when they’re like, oh my gosh, you’re so excited about this. But gosh, you never said anything about your other one. That’s you kind of get a sense of like what is building up to be your career. And so it’s not a great answer, but it was a culmination of things that, you know. The culture, the people, the mentorship, the operations. I mean, everything kind of came together for me.
36:35 Closing: What is One Thing that Brought You Joy Today?
Annie: That’s a fantastic answer. your passion is still so alive and it’s like coming at me in the screen. And I really appreciate that. And this is the a small thing that I like to do with all of our speakers. But the, the actual final note is, what is one thing that brought you joy today,
Dr. Park: Talking to you guys like, I feel like I’m looking at myself, like, you know, 15 years ago. And I wish that I had someone who looked like me that could be telling me this, because then I would feel more comfortable thinking about this path, and not that I was ever really scared, but it took me more time than it should have. And I think if I had seen more mentors who were women, who were surgeons, I don’t I feel like it would have been more clear for me. Um, I don’t regret at all the path that I took because I learned so many things along the way. But I mean, who knows? You guys are so great, and, I’m so excited that you guys are excited about this, too.
Annie: We appreciate that so much. And just for context, for everyone on the call. We actually found Dr. Park through, a leadership committee event last year. It was ‘Preparing for PGY1’, I believe. And you actually met, Dr. Nolan Kagetsu. And he brought you on, and you were so excited to find an organization like APAMSA that was dedicated to this effort. and you’ve been so excited to help us ever since. So, from the bottom of my heart, we really do appreciate your willingness to be here. And thank you so much for all of your insights today.
Dr. Park: Of course, of course.
Annie: So that concludes our September AMA session. Thank you to everyone who attended and for everyone who’s going to listen on the podcast. Please reach out if you have any questions and we really appreciate it. So last round of applause for Doctor Park.
Dr. Park: Thank you guys.
Episode 1 - A Conversation with Victoria Shi

Listen here:
YouTube
Spotify
Apple Podcasts
This episode was produced by James ‘Jameson’ Chua and Ashley Tam, hosted by James ‘Jameson’ Chua, and graphic by Callista Wu and Claire Sun.
Chapters and Timestamps
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
00:38 Introduction to Victoria Shi
03:39 How and why did you get involved with APAMSA?
05:21 APAMSA accomplishments and highlights
07:06 Impact of mentorship in medicine
08:32 APAMSA role models
10:09 Upcoming events and APAMSA’s National Conference
12:05 Leadership in APAMSA
13:27 Creating initiatives and collaboration in APAMSA National Board
15:24 Advice for attending medical conferences alone
17:30 Choosing Dermatology as a speciality & residency applications
19:49 Dermatology research fellowship
21:11 Dermatology research conferences
21:53 Subspecialties within Dermatology
23:28 Skincare & other misconceptions in Dermatology
25:14 What are you looking forward to in your medical career?
26:22 Relocating for residency and beyond
27:02 Philadelphia & city life
31:23 Rapid fire getting-to-know-you questions
34:08 Advice for pre-medical and medical students
00:00 Introduction to White Coats & Rice: An APAMSA Podcast
James: Welcome everyone to the first episode of the Asian Pacific American Medical Student Association Podcast. As a brief introduction to this pod, we have so many things in store for you for future episodes. From roundtable discussions of current health topics, to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization. This is White Coats and Rice. My name is James Chua, second year medical student at Touro University Nevada College of Osteopathic Medicine and the current Fundraising Director at APAMSA. I’ll be your host today and one of the rotating hosts throughout the podcast’s various episode styles.
00:38 Introduction to Victoria Shi
James: On today’s episode, we have with us Victoria Shi, a fourth year medical student at the University of Missouri Kansas City School of Medicine. Victoria is an R&B music lover, coffee enthusiast, and most recently a passionate home cook who specializes in one pot budget friendly meals. Victoria has been on a remarkable journey in medicine. Most recently, she’s been immersed in a year long dermatology research fellowship at Northwestern, expanding her expertise and making strides in a field that she’s passionate about. In 2018, to better connect more deeply with her AANHPI roots, she joined the Asian Pacific American Medical Student Association. Over the last six years, Victoria has become a dedicated leader within the org, serving in multiple roles such as a local chapter president, Region 6 director, alumni co-director, strategy vice president, and now as APAMSA’s national president. In her role, Victoria is committed to building connections between APAMSA’s local chapters, amplifying the voices of underrepresented AANHPI communities, and championing health literacy, and research initiatives. Through her work, she’s found a strong sense of community and joy in uplifting and supporting others. Outside of her studies and advocacy, you’ll likely find Victoria traveling, exploring nature, diving into the food scene in new cities, or enjoying her hobby of cooking and baking. Join us as we dive deeper into her journey, passions, and goals for the future. That was taken out of your bio, if that sounds familiar.
Victoria: Thanks, James, for that introduction. I was like, you’ve done your research. That’s my APAMSA CV right there. I’m honored to be here for the first episode of our APAMSA podcast. Yeah, just happy to be here.
James: Yeah, we’re happy to have you and we cannot thank you enough for being our first guest. I think we have a bunch of questions so our listeners can get to know you better. But I think the most important question of all is, how are we doing today?
Victoria: We’re doing wonderful. We got off an EM shift and yeah.
James: That’s awesome. I haven’t started the battle of rotations and stuff so I can only imagine how tired you must be, but we are very grateful for you to take the time out of your day to be our first guest.
Victoria: I’m happy to be here. I think you’ll enjoy it. I think rotations are just very rewarding. I mean, even if you come home at the end of the day tired, you’re like today I was like immersed in patient care, and just in the thick of it. So I really enjoy the tired when I come back from rotations.
03:39 How and why did you get involved with APAMSA?
James: That’s awesome and really inspiring and I can’t wait to dive more into that. But some of these questions we have, but I think since this whole organization is focused on like, AANHPI healthcare and stuff. I’m just really interested. So six years in APAMSA, right? Why did you join the organization in the first place?
Victoria: Yeah, one of my factors when first getting started with APAMSA is I was really searching for an Asian community when I started my undergrad and into med school. I grew up in Pennsylvania in like Southeastern Pennsylvania. It wasn’t very diverse at all. I was one of the very few Asian Americans in my grade. So when I came to undergrad, and so I did a joint undergrad and med school program. So when I came to UMKC, I saw that we have an organization of APAMSA that celebrates diversity, and people are really, really like, they’re proud of their heritage. And that’s why I initially joined. But after being involved in it for the past six years, I feel like I’ve really found my, like a second family here. I found a community, and that’s what kept bringing me back. We, with the local chapter members, with the national APAMSA family – it just felt like a second home. I also loved our mission too, like on a local scale, whether that’s, it’s just giving back to the AANHPI community. So whether that’s helping with health fairs on a local level, or doing screening events, and then on a national scale, really bringing together the diverse communities, celebrating all the diverse voices, and also just advocating for AANHPI health on a broader scale.
05:21 APAMSA accomplishments and highlights
James: That’s amazing. I mean, with six years of experience, like, what would you say is the most standout thing to you, like that you have done so far? Like when you look back during your time, or maybe even like during residency interviews, like this is the one thing you are definitely going to share with everyone.
Victoria: I think I would say the mentorship programs that we’ve started and carried through. I think one thing, like even amongst all our goals of advocating for health equity, and advancing the health Asian and AANHPI communities, I think what stands out to me is that mentorship runs deep, whether it’s from the alumni to the medical students, the medical students to the pre med students. We’ve, for example, established our big sibling, little sibling program, where we have our national board members mentor pre meds. We also have our like ERAS and residency application programs to help our medical students transition into residency. So amongst all of this, I think what I’m most proud of is that we’re really extending our hand out to the future leaders, the future medical students, the future health professions. And we’re really lifting them up and making them into better, better carers, better providers in the future. And I think that will in and of itself help make for a better patient population.
07:06 Impact of mentorship in medicine
James: Absolutely. It’s definitely that like pay it forward mentality. You know, it’s like, what can I do right now to give back to the future? And I remember like, even in my own experiences, like, I never really got it at first. Why my mentors were always so like, eager to help me, you know, but then they really painted it, you know, they’re like one day if like what I’m doing for you right now helps you make like huge waves in the healthcare community, like whatever position you end up as like, that would be worth it.
Victoria: I agree, I don’t think I would not be like where I am today without all the help of my mentors, and there’s many of them. I when people say it really takes a village now sitting on the other side as a fourth year medical student, you know, applying to residency about to, I mean, about to graduate in a matter of months, I am really thinking back and reflecting on how many people have helped me along the way. There’s been physician mentors, I’ve had there’s been other medical students, other peers, even those in the grades before me, who’ve helped me in all different aspects, whether it was school, whether it was getting involved in leadership organizations, whether it was like getting involved in advocacy, just, you know, guiding me through rotations. So when I look back, there’s definitely a village supporting me and I think that’s what makes me want to pay it forward and help others as well.
08:32 APAMSA role models
James: Would you say there’s somebody like either like a board member from APAMSA or maybe like one of the alumni, like one person you could give a special shout out and talk about your experience with them and how they’ve impacted you?
Victoria: Honestly, there’s been many. I’ve been inspired by all the past presidents, you know, Joyce, Donna, Yingfei, these were all the presidents at some point while I was on board. And I think really seeing their leadership, seeing how much they care about APAMSA and their dedication really inspired me to go forward. But honestly, every national board member that I’ve worked with has inspired me too. Just seeing them like work so hard on their own initiatives, come up with new ideas, make new advances has been inspiring as well.
James: Absolutely.
Victoria: There’s too many. I would spend way too long if I was listing all the people that inspired me.
James: Definitely. I will say, you know, as a director myself, you have definitely inspired my work.
Victoria: Thank you so much. You’re literally doing so much for like we’re just excited by all the new initiatives you have like all the streaming tournaments you’ve had like adding all our merch up, like you’ve done so much as fundraising director and we’re all very proud of you.
10:09 Upcoming events and APAMSA’s National Conference
James: Thank you. Yeah, there’s a lot more in store. Our tenure is like four months left or so for elections. And on that note, is there any like inside scoop you could give our listeners to what we could expect within the next four months? Within the last four months of your presidency? Any new cool things happening in the horizon?
Victoria: I think everyone can expect in the next couple months, we are having our national conference, the first weekend of March in 2025. This will be at Duke. Super excited. The national conference directors have been working hard on this. We have all our speakers lined up and just be on the lookout for the speaker lineup to be posted.
James: Definitely. Yeah, this would be actually my first national conference. I had tickets or I had a ticket to the UNLV conference last year, but I was a little too… I was um, I was a little too shy to go because this would be my first medical conference and I was under the impression that no one from my APAMSA or no one from my medical school would be going. Okay. And so I just didn’t go because I was too shy and like too nervous. Right.
Victoria: What did you do with the tickets?
James: Well, I just had it. I just sort of kept it. But then by the end of the night, all of a sudden I started getting like texts and like Instagram DMs like saying congratulations, but no context. I was like, what’s happening? Did I win the lottery? I was like, what am I missing? And then finally someone like provided context. They were like, oh, you won your position for fundraising director in APAMSA. And then I realized that’s even better than winning the lottery.
Victoria: Awww, that’s so sweet. Were you, were you expecting that? Like was that totally out of left field for you?
12:05 Leadership in APAMSA
James: Right, inside scoop. So when I applied, so for my medical school personal statement, I like talk so much and touch upon so much about the importance of AANHPI healthcare or health disparities and like wanting to improve upon that, you know, like I feel like that’s the dream for so many of us as Asian, Asian Americans. And so I just really, this organization in particular, either at a local level or on a national level, it was my goal to be a leader in some shape or form, you know, like right away I immediately like became the local chapter president at my medical school. But when I applied to the national board, I like had no expectations. And also like if you go back and rewatch that video, there’s a particular like hoarseness to my voice because I actually recorded it while I had strep throat.
Victoria: The dedication.
James: Yeah, but I knew I wanted to apply, you know, and there was actually like, I felt like for me personally in the skillset I bring in my personal background, there was not another position I felt more comfortable for, you know. And so that’s why I sort of just like threw all my marbles in at that one position and here we are. Yeah.
13:27 Creating initiatives and collaboration in APAMSA National Board
Victoria: How have you felt like it’s been for you this year? I feel like harder than expected, like how has it been coming up with the fundraising ideas and you know, having that creative side.
James: You know I, one, I think it was a lot easier than I thought it was going to be. I think it’s just it is because, you know, you and Wendy, the External Affairs Vice President, my VP. You guys give me so much leeway and so much freedom to do whatever it is that I want to do to help APAMSA to help raise money and all this and that. So that’s, that’s the easy part, you know. But since I lack creativity, especially when it comes to designs and stuff for the merch, the storefront, that’s why that could be a challenging part for our listener who may want to become the next fundraising director, you know. But having a team behind us, like having that sense of like camaraderie or that sense of teamwork with other board members who have that more creative side to them, you know, like that’s what made my job so much more fruitful than I could ever imagine it to be. And I feel like I don’t know if this position is like really designed in such a way to be so collaborative, but being able to be so flexible in that way, you know, like always like DMing other board members on Slack. Like that’s what really has brought so much fun and so much joy. And like the reason why I want to keep on joining APAMSA because we have like leaders like you making it such like a homey environment or such a familial environment. So yeah, so for any listener who may be interested in joining APAMSA, I would say, yeah, just apply for it, you know, elections in March, lots of positions. We will definitely, we’ll find a space for you. But I have a question for you then. So since you now have heard my story that I was too shy to go to the conference by myself, have you ever gone to a medical conference by yourself or do you have any advice for somebody who is like considering going to one? Being nervous about it?
15:24 Advice for attending medical conferences alone
Victoria: Let me think. Have I gone to one by myself? I at least for the APAMSA ones, we always go, I’ve at least had a few chapter members with me and these days since I’ve been in a APAMSA for so long, it feels like there’s lots and lots of friends there. But I think if you’re attending a medical conference by yourself, don’t be afraid. My advice to you would be everyone like everyone there, the students, they want to connect with other people and there’s lots of other students who are also attending by themselves and want a buddy. So my advice to you would be to go to the breakfast, the lunchtime, the networking sessions, especially amongst the attendees. And if you just chat up the person next to you, 90% of the time, will have a buddy for the rest of the conference. So I think just shaking off the nerves and knowing that people there want to connect with others is very, very helpful. But I’ve experienced the same thing, especially if I’m networking at a conference and there’s someone like an attending or something that I’ve heard a lot about or I’m interested in their research and I want to talk to them, I always get that nervous pit in my stomach too before approaching. Sometimes I just have to make myself do it.
17:30 Choosing Dermatology as a speciality & residency applications
James: Right. Absolutely. And I think that actually is a really good segue into our next topic. Like you know, you have been to research conferences, you have done that networking and I feel like when you’re applying to residency, like that networking and forming those connections, it’s so important. You know, having the right connections can score you the most amazing residency. And on that note, like since you’re a fourth year, have you decided what field of medicine or what specialty of medicine you’re most interested in is yet?
Victoria: I actually applied dermatology this past cycle. So we’re currently in the midst of doing interviews. Still, we interview a little bit late, so we’re still receiving them and a lot of them are scheduled for, you know, December, January, even into February.
James: Yeah. How did you choose dermatology? So you’re a fourth year, at what point in your medical career did you realize like, oh man, like Derm is the one for me, you know?
Victoria: So I realized during second year, we have a free dermatology clinic in Kansas City and I really fell in love when with Derm, when I started volunteering there, I got to see kind of the procedural side of it. I got to see, it’s very, it’s very dynamic specialty. In my opinion, you have to be like, think quickly on your feet. There’s always a lot going on and I really love that about it. But what really sold it for me was this free Derm clinic, we see a lot of underserved patients. A lot of them have really severe skin disease. So I saw how much we’re able to help them, especially that patient population. And I really saw the disparities, the socioeconomic disparities kind of manifest in skin disease. And one thing that I think that I found super special was that we have lots of creative options to help these patients. So this free Derm clinic, we have a special 340B pharmacy. We’re able to get them biologics for like $4 a month, like patients who otherwise wouldn’t be able to afford it. That’s really when I fell in love with Derm, but then I waited until I was done with all my clerkships third year and I still felt that Derm was for me. So that’s when I knew for sure.
James: Yeah, that’s awesome. You must be one very hardworking student because I know how difficult it may be to land a dermatology residency.
Victoria: Fingers crossed. Fingers crossed.
19:49 Dermatology research fellowship
James: No, we believe in you. We’re all listening. All of the listeners, we believe in you. So you also did a one year fellowship, dermatology research fellowship, right? Could you tell us more about that?
Victoria: Yeah, so I did this at Northwestern and my research mainly focused on developing guidelines within dermatology and it involved a lot of multidisciplinary work as well. But I really worked on a few, like for example, guidelines for when to do cosmetic procedures in minors. And it was a multidisciplinary offer of plastic surgeons, pediatric subspecialties, there’s
dermatologists, dermatologic surgeons, medical ethicists. So I really loved working with these different specialties, different groups of people and kind of, I felt some agency in my research getting to really convene the panel, do the literature search, bring the experts together and have them meet consensus and then kind of finalize the guidelines. So just loved the process, love that we’re able to standardize care.
21:11 Dermatology research conferences
James: Has your work brought you to like any cool conferences? Like have you been all over the US for it yet?
Victoria: Actually, I feel very fortunate. I was able to go to quite a few conferences during my research year. So I went to AAD, that’s American Academy of Dermatology. That was in San Diego. I was able to go to the American College of Mohs Surgeons conference in Arizona. I went to the American Society of Lasers in Medical Science. That was in Baltimore. So really did get to travel all over and I’m very, very grateful for that. Met a lot of people, heard a lot of interesting research as well. Very rewarding.
21:53 Subspecialties within Dermatology
James: Definitely. And then you touched on seeing like a variety of different like dermatology, like folks who like specialize in different fields of dermatology, right? Do you know like if you want to subspecialize within dermatology or, because to be honest, like as for me as a second year, I haven’t even gotten close to anything Derm and then also I’m in my little bubble of like, I want to be a future psychiatrist. So I really yeah, so I have really no idea what’s going on in Derm.
Victoria: I’m still undecided. I’m kind of keeping my mind open and I think I’ll decide once I get a little bit more exposure to Derm. But as far as topics within Derm that interest me, I do think medical dermatology, like all the systemic diseases like lupus, scleroderma, like all the skin diseases that have systemic organ manifestations, that stuff interests me because there’s like a lot of, I don’t know, like a lot of the treatments for that are super complicated. You have to be like pretty experimental. So that’s something I’m interested in. I’m not sure yet. As far as the different specialties within Derm, we have Mohs surgery, we have peds Derm, we have dermatopathology, and I think it’s like 50/50 whether people split or not. Like some people just practice gen-derm and others like go on to do fellowship. So undecided, keeping my mind open.
23:28 Skincare & other misconceptions in Dermatology
James: So is there, and so I know skincare is like a huge part of Derm. Is there one misconception, not it doesn’t have to be about skincare, I guess, but like just in general, is there one misconception do you think that you would like to correct upon that many people have about the field of either dermatology or if you want to go very specifically about skincare? Because that’s something everyone can relate to, you know, or like any words of wisdom you have that really should be shared.
Victoria: I think one misconception that people have is that dermatologists just treat acne. They just do cosmetic treatments. It’s all about like looks. And while that there is like a subspecialty of Derm that is cosmetics, the majority of the time we do kind of like I was saying about medical dermatology, Derm is like the intersection of many specialties. We have the opportunity to work closely with rheumatology, say if our patients have inflammatory arthritis like psoriatic arthritis, we have the opportunity to work with allergy, like if patients have like an eczema allergy overlap. So we really are also like a very medical specialty as well. And it’s not just about appearances. We also really help patients in that sense.
25:14 What are you looking forward to in your medical career?
James: Yeah, absolutely. Thank you for clearing that up. That is also, I don’t want to say I’ve had that misconception, but you know, I’ve had that thought. But so since residency is in your near future, just right around the corner, I think that leads us to our final topic. And that’s what is something you look forward to in your medical career?
Victoria: I think I really look forward to working in the specialty that I’m interested in. I’m just excited. I’m already envisioning myself as a resident, young attending, getting to start and build those longitudinal relationships with patients. I think that’s so special. One of the reasons I was drawn to medicine in the first place, but I’ve, I’ve been in work with some dermatologists who’ve treated patients from like childhood all the way into adulthood. And that’s so special. I want the same thing. One other thing that I’m really excited to do, we also, we touched a little bit about
this earlier. I’m really excited to work in a mentorship role with medical students and residents. I’ve loved all the opportunities that I’ve had to, you know, work in that capacity. And just excited to like have a career and incorporate teaching in that.
26:22 Relocating for residency and beyond
James: Do you think would you ever go back to South Pennsylvania? South is it or East? Near Philly is what I’m asking.
Victoria: Oh yeah, for sure. I think I’m pretty much open to ending up wherever I do think like the Northeast has this special place in my heart, just cause you know, family’s close by. I really think of myself as a city girl, but after living in the Midwest for six years, I also really like it. So I’d be happy to go anywhere. We’ll find out in March.
James: Definitely. I actually, I don’t have like the exact same trajectory as you, but so for me myself, I grew up in Southern California, right? Okay. So before matriculating into medical school, I was in Philadelphia for two years. Like I was like, I was in center city and like, even so whenever somebody asks me where I’m from or what’s my hometown, I always have to say, yeah, I’m from San Diego and they’re like, oh, so great. But I’m like, no, but I love Philly. I love the city life and that’s like what I am like trying my best to work so hard for so I could place like land a residency in some big city, you know.
27:02 Philadelphia & city life
Victoria: What was like, what were you working in Philly at the time? And also what was your favorite part about living there?
James: Oh, so I moved there to do a post-bac. And so I did Drexel University’s one year special master’s program. And then by the end of the year, I got into a medical school and then I would, but they didn’t let me know until June. And I was like, hmm, with it being Touro, Nevada, I was like, so in other words, I have to pack up my whole life in less than a month, like find roommates, find housing, you know, figure out everything. It was like, or I could just stay in Philly for another year. And so during that bonus year, my like finally free gap year where I wasn’t studying for the MCAT, where I wasn’t studying for classes, where I was just living my life, I worked for Johnson & Johnson as a scientific writer. And so that was really fun seeing the more like seeing the more industry side of medicine and research, you know. And so what I miss most about Philly and what I think really just draws me to city life in general is that, so I lived in like truly the heart of Center City of like Philly, Philly. And so for folks who are like really familiar with Philadelphia, for our listeners who are like from that area, I lived like essentially in Rittenhouse square, you know, so like Chestnut and like whatever, you know, central number, right. And so being able to wake up and then just take the elevator down and walk across the way to like some coffee shop, like being so accessible, everything via walking, you know, and being able to see like the same regular faces throughout the time, like of living in the city, like that’s what made it feel like home despite the hustle and bustle of the city. I feel like that may not be, at least in my experience with something like, you know, Manhattan, like that is such a transient city. Like people are constantly like in and out. Whereas like Philly, like people just live there, you know.
Victoria: Yeah.
James: So I really miss that aspect of just public transport being able to walk everywhere. You know, I remember like living in San Diego or living in Las Vegas, right. There will be a like, we’ll be parked at like a restaurant, like, oh, let’s grab Korean barbecue, right. And then we’ll be like, oh, y’all all down for boba, right. And then it’ll, I’m like, oh, the boba shops a block away, right. And then everybody walks towards their car. And I’m like, you guys, it’s like a three minute walk. And they’re like, oh, it’s a one minute drive. And I’m like, oh, my gosh, guys, I get it though. Yeah.
Victoria: I’ve seen, I feel the same way because I’ve seen both sides in Kansas City. We drive everywhere. So you get kind of spoiled. Like all you have to do is walk not even a hundred feet to your car and you have access to everywhere. But I will say when I was doing rotations in New York, when I was exploring New York, I just love like you get 10,000 steps a day, probably more if you’re exploring out 20,000 steps. So there’s nothing healthier than like living in a city and walking everywhere.
31:23 Rapid fire getting-to-know-you questions
James: Yeah, absolutely. Yeah. So fingers crossed, let’s end up somewhere great. Absolutely. So that pretty much wraps up all of our main topic questions. So we’re going to end our little podcast with a quickrapid fire questions of this or that questions. Okay. So it’s either A or B and just a silly last minute way to get to know you.
Victoria: You know, I’m so indecisive. So this is going to be, this is going to be hard.
James: Like pretty simple. Okay. It’s pretty like your heart will ust speak for itself. You know? All right. You ready? Yes. All right. I think we know the answer to this one, but city or beach.
Victoria: City
James: Cats or dogs.
Victoria: Definitely dogs. There’s so I’m also allergic to cats. So that was an easy one.
James: Text or call?
Victoria: Call
James: Black or white?
Victoria: Black.
James: Morning or night?
Victoria: Hmm. Definitely a night person. I’m a night owl.
James: Nice. Summer or winter.
Victoria: Summer.
James: I can see that coming from the Northeast. Breakfast or dinner.
Victoria: Love breakfast. Actually brunch is my favorite meal. Eggs, eggs, potatoes. Amazing.
James: Would you rather have the power to be invisible or the power to read minds?
Victoria: I think I like to be invisible. Sometimes you just don’t want to be perceived. And also I think if I have the ability to read minds, it would just be so overwhelming. Just thoughts coming at me from everywhere.
James: Definitely. And then last two questions. Would you rather have $100,000 to spend on yourself or have a million you can only spend on others?
Victoria: I would have a million dollars to spend on others. Just so much more we could do with that.
James: Definitely. And then for our last this or that question, would you rather retake step one or retake the MCAT?
Victoria: Fun fact. So I have never taken the MCAT because our school, the six year program, we don’t have to take that. So I don’t know what that’s like, but I will. But we’ll say I would take that.
James: Take the MCAT?
Victoria: Take the MCAT.
James: Well, that’s a good plug.
Victoria: Yeah. Have you taken step one yet?
James: No, I haven’t.
Victoria: You should survey. I want to see what other people say to that.
34:08 Advice for pre-medical and medical students
James: Yeah. I will let you know for our next – I’ll say this is what Vic said. Well, in that case, that wraps up our this-or-that question. Thank you for your candid honesty. We would like to end the first episode of White Coats and Rice with seeking out advice from you. So what is one piece of advice you’d like to offer someone who’s, you know, either a pre-med or medical student who dreams of getting into medical school or even more importantly, you know, getting to the finish line slash where you’re at as a fourth year medical student?
Victoria: I would say that really trust your own journey. Everyone’s journey is going to be different. If you ask a hundred medical students, all of them will have had different experiences
with whether they took gap years or not, what they did during their gap years, even their journey throughout medical school. So I think one of the biggest things I would say is to stop comparing yourself to others and really trust your own journey. And I heard this quote once and it really stuck with me or more just a way of thinking about things. So one, a resident, I think I heard this on a podcast. She said, “pretend like you’re driving a car, the destination where you want to go, you put that into the GPS, you’re going to get there. Now it’s all about really enjoying the journey itself.” So that really stuck with me. No matter what, like whether your goal right now is to get into medical school or your goal is like, you’re currently thick of applying to residency and you want to get into your dream residency, you’ve already put the destination to your GPS. You’re going to get there. Now it’s about just doing the driving.
James: Definitely. Yeah, that as a second year and as a, you know, somebody who wants to be on like higher leadership of APAMSA, that is definitely something I needed to hear right now. So thank you, Vic, for sharing that.
Victoria: Your destination, Philly.
James: Absolutely. Okay. Well, all right, everyone. That is our APAMSA President, Victoria Shi.
If you have any questions or want to reach out, feel free to email her at president@apamsa.org. Victoria, Vic, it’s been such a pleasure getting to know you better. And we’re so grateful for you for being our first guest on White Coats and Rice. Thank you for sharing your story and inspiring all of us.
Victoria: Thanks so much for having me. First podcast down for me too.
James: As I know, first of many, I’m sure in the future we will definitely be inviting you
to hear more about your story.
Victoria: Thanks, James.
James: Of course to our listeners, we hope you enjoyed today’s episode as much as we did. Don’t forget to tune in next time. And until then take care and keep striving. Catch you all soon. Thank you.
Navigating the Intersectional Bamboo and Glass Ceilings: Empowering Asian American Women in Medical Leadership
Leadership is crucial in medicine, yet it often takes a backseat to technical and academic training. For underrepresented groups in medicine, additional challenges including historical discrimination and stereotypes hinder leadership development even further. Asian Americans in medical leadership are impacted by the phenomenon called the “bamboo ceiling,” which refers to the multifaceted challenges (ranging from cultural differences, systemic bias, ingrained stereotypes, and lack of role models) that prevent Asian Americans from achieving leadership positions. More specifically, Asian American women in particular are challenged by a double ceiling effect by having to overcome both the bamboo ceiling and the glass ceiling (social barrier that prevents women from workforce advancement).
Initially, we wrote these five tips to help Asian American women at any stage of their career to navigate the challenges in developing leadership skills and promoting inclusivity in medical leadership. However, we believe these tips are helpful for all individuals, especially those underrepresented in medicine, looking to advance their leadership skills and enhance allyship in medicine.
Tip 1 – Practice public speaking
Every time I am about to present my patient, no matter how effectively I have pre-charted, my heart rate rises and my hands get clammy. After speaking to some of my residents, I realized the fear of public speaking is nearly universal. And while TEDx speakers seem calm and collected, I have learned that hours of practice and coaching produce those talks we enjoy watching.
Public speaking is a skill that takes time to develop. Take advantage of everyday opportunities, like teaching medical students or presenting at noon conferences or journal clubs, to become more comfortable in front of an audience. Raising the volume of your voice and straightening your posture can also project an air of confidence. Ultimately, what helps calm me down the most is imagining myself having a conversation with a friend and telling a story – about a patient, physiological processes, research – and it becomes more manageable.
Tip 2 – Identify mentors, build relationships, and network with others
Becoming a leader does not only involve yourself; the process humbly involves a team of people who invest in and support your endeavors. Finding your team may seem daunting with various clinical environments, hierarchies in medicine, or perhaps feeling shy or burdensome when approaching potential mentors. However, one such skill to build your network is through learning how to engage in conversations with people from all walks of life. To start, ask about others’ interests and backgrounds to explore commonalities unveiled through conversation. We also find it easy to stimulate discussions with questions such as, “What is an exciting project you are working on?” or “What are your thoughts on [blank] event?”. We also recommend preparing a short 30-second elevator pitch of yourself (your educational background, interests, and goals) to use in the appropriate settings. These conversations may not seem natural at first. However, by practicing with each social opportunity you may have, you will feel more comfortable to humbly approach others and form new relationships.
One fortuitous experience I had was going to a medical conference across the country initially not knowing anyone. I remember grabbing a bagel from the breakfast station and saw another woman sitting nearby and eating alone. I decided to strike up a conversation in hopes of building a connection and friendship. We became friends and, to this day (although living many miles apart), have continued to support one another while working on projects and holding leadership roles in the same Asian American organization.
Tip 3 – Resolve conflicts when necessary
When it comes to conflict resolution, many individuals may struggle with the internal monologue, “Do I speak up? Or, do I keep my head down and stay quiet?” On one hand, many – especially Asian American women – have grown up with the virtue of humility, to “not rock the boat” and take a back seat. However, learning the art of conflict resolution is important and necessary to not only pave the wave for smooth relationships but also can influence team dynamics in the future. Here are some steps that I take to ease my stress before I manage conflict:
- Address the issue early
- Find the right place and right time to converse honestly with the other party
- Use AEIOU (Acknowledge, Express, Identify, Outcome, Understanding)
- I find it helpful to use “I feel/think…” statements to clarify how I feel I have been impacted. Use non-defensive phrases like “I would like…” instead of “I want…”.
- Overall, I try to keep a calm mind and separate the person from the problem.
Tip 4 – Ask for what you deserve and be aware that negotiation is a process
While negotiating a salary may seem more relevant after residency, try to consistently check in with yourself on your short-term and long-term career goals to see if the trajectory you are on will meet them. Also, understand that business is not always a meritocracy. You may be a diligent and hard worker, but you may be selling yourself short by not asking for the compensation or promotions you deserve.
Some actionable items that you can consider doing are recognizing the skills you bring to a team and the deliverables you have produced. Do research on the current job market to know the ballpark range you should be negotiating within. And be patient, as negotiation is a dance between two parties and takes time. Bottom line: Ask or you don’t get, and do not sign the first contract you see!
Tip 5 – Find your work style and that of your colleagues
Understanding you and your colleagues’ work styles can help improve synergy between one another. While there are multiple personality assessment tools, I like to use the “Five-Factor model of personality”, which helps ascertain how you score on each of the Big Five (OCEAN: Openness, Conscientiousness, Extroversion, Agreeableness, Neuroticism) personality traits. Finding your work style is important for self-reflection. It can be invaluable in knowing your boundaries, especially when it comes to learning when to say “yes” and how to say “no.” And, personality tests can be used as a team-building exercise. As a peer, knowing your colleagues’ work styles can be essential to learn how to collaborate effectively with one another. As a leader, learning your colleagues’ work styles can help assign team roles, set expectations, leverage strengths, and cater to individual work styles.
Conclusion
To the AAWM and individuals reading these tips, we hope that these tips and references provide great resources to help you succeed in your medical career and develop your personal leadership style. Ultimately, we hope that the medical community can come together to break through systemic barriers and cultivate diverse, equitable leadership that enhances patient care and drives positive healthcare outcomes.
Written by APAMSA National Board Members: Sonia K. Scallon, MD; Ellis Jang, BS; Victoria V. Nguyen, BS; Sunny S. Park, MD, MPH; Cynthia X. Pan, MD
A prescription from the next generation of doctors: Vote early
As future medical professionals, we see the real-life consequences of political decisions in emergency rooms, hospitals, and clinics. Despite a growing recognition that voting is directly linked to better health outcomes, however, health professionals are voting at lower rates than the national average. It’s time that we make a change this election.
We see patients denied essential services due to bureaucratic hurdles, such as insurance coverage gaps for life-saving medications or underfunded social and mental health service programs. As medical students and leaders of health in our communities, we have a responsibility to vote—not just for ourselves but for the people we serve.
The American Medical Association (AMA) recognizes voting as a social determinant of health. Communities with higher voter turnout often experience better health outcomes, yet many health care providers, including medical students, face challenges in turning out to vote. Busy schedules, unexpected emergencies, and the demands of our profession can create real barriers. We must break this cycle, and the remedy is early voting. By casting our ballots ahead of time, we can ensure that our voices are heard to better the health of our communities and patients.
Many of us have celebrated our family members finally gaining citizenship, only to see them struggle within a health care system full of obstacles. These are not isolated incidents; they reflect the broader experiences of disinvested communities whose voice at the ballot box can have a meaningful impact. The Asian American, Native Hawaiian, and Pacific Islander (AANHPI) communities face the brunt of harmful anti-immigrant narratives, echoing xenophobic sentiments that have long afflicted our communities that contribute to social isolation and negative health outcomes.
Yet, AANHPI advocacy has a rich history in the United States—from Japanese American activist Yuri Kochiyama, who fought for civil rights alongside Black leaders, to Native Hawaiian scholar Haunani-Kay Trask, who advocated for Indigenous sovereignty. In honoring their legacies, we recognize that voting is one of the most powerful tools we have to shape healthier communities and, in turn, a healthier democracy.
At the Asian Pacific American Medical Student Association (APAMSA), the largest student organization of AANHPI medical students and pre-medical students, we’ve made civic engagement a priority this year. Partnering with the non-partisan, non-profit organization Vot-ER we’ve implemented training among our over 4,000 members and participated in programs to help medical professionals get ready to vote and help their patients to vote. Today, we are calling on medical students and professionals, particularly within the AANHPI community and beyond, to close our voter turnout gap by voting early.
Health is always on the ballot, and this election provides a critical opportunity to create a health care system that works for everyone. By voting early, we take an essential first step toward realizing that vision of healthier and more equitable communities. Our role as future physicians extends beyond the clinic walls. During this election season, we must show up—not just for ourselves, but also for our patients and communities. Let’s ensure that our voices are heard by voting early in this and every election.
Make your early voting plan today.
Alexander Le, Annie Yao, and Victoria Shi are medical students.
Find the original posted OpEd here.
Ask Internal Medicine Physician Dr. Marcus Iwane
The Leadership Committee proudly presents Dr. Marcus Iwane, an internal medicine physician dedicated to cultural health and Hawaiian communities. With a deep understanding of the intersection between medicine and heritage, Dr. Iwane is dedicated to ensuring that future generations continue to thrive while honoring their roots. His other passions include fishing, farming, and traveling!
Join us October 3rd for an exclusive Ask Me Anything session where Dr. Iwane will share his insights on health, culture, and the importance of community care. Don’t miss it!
Zoom Meeting ID: 952 5920 8549
Region VIII Conference
APAMSA Region VIII and the UCI APAMSA chapter are ecstatic to invite you to the annual Region VIII Conference hosted at the University of California, Irvine in Irvine. We are excited to host this event, celebrate all backgrounds, and uplift AANHPI communities through our conference “Turning the Tide.” Our theme highlights the shift in narrative towards unity, commemorating diverse backgrounds and perspectives, and acceptance of all. Through this conference, we hope to uphold this goal by hosting influential speakers in the AANHPI sphere, facilitating pre-medical and resident/attending panels, and featuring the research contributions of APAMSA members.