Jerry Cui, Alumni Co-Director
Network Director
I am a 6th year MD/PhD student at Ohio State. I grew up in Charlotte, North Carolina and graduated from Yale in 2016. My research focuses on discovering bacterial natural products and elucidating their biosynthesis in an effort to develop novel therapeutics. I’ve served as one of the APAMSA Alumni Directors for the past few–probably too many–years.
Janet Guo, Academic Education and Research Director

Network Director
Janet Guo originally hails from Lexington, KY and is now a medical student at the Warren Alpert Medical School of Brown University. She is thrilled to serve as the Research Director for APAMSA. In her free time, Janet enjoys exploring bubble tea shops and practicing yoga.
Want to host the 2024 National Conference?
Interested in hosting our 2024 National Conference?
Head over here to learn more!
We will be hosting an open Q&A on March 22, 2023 at 7pm EST – 8 pm EST
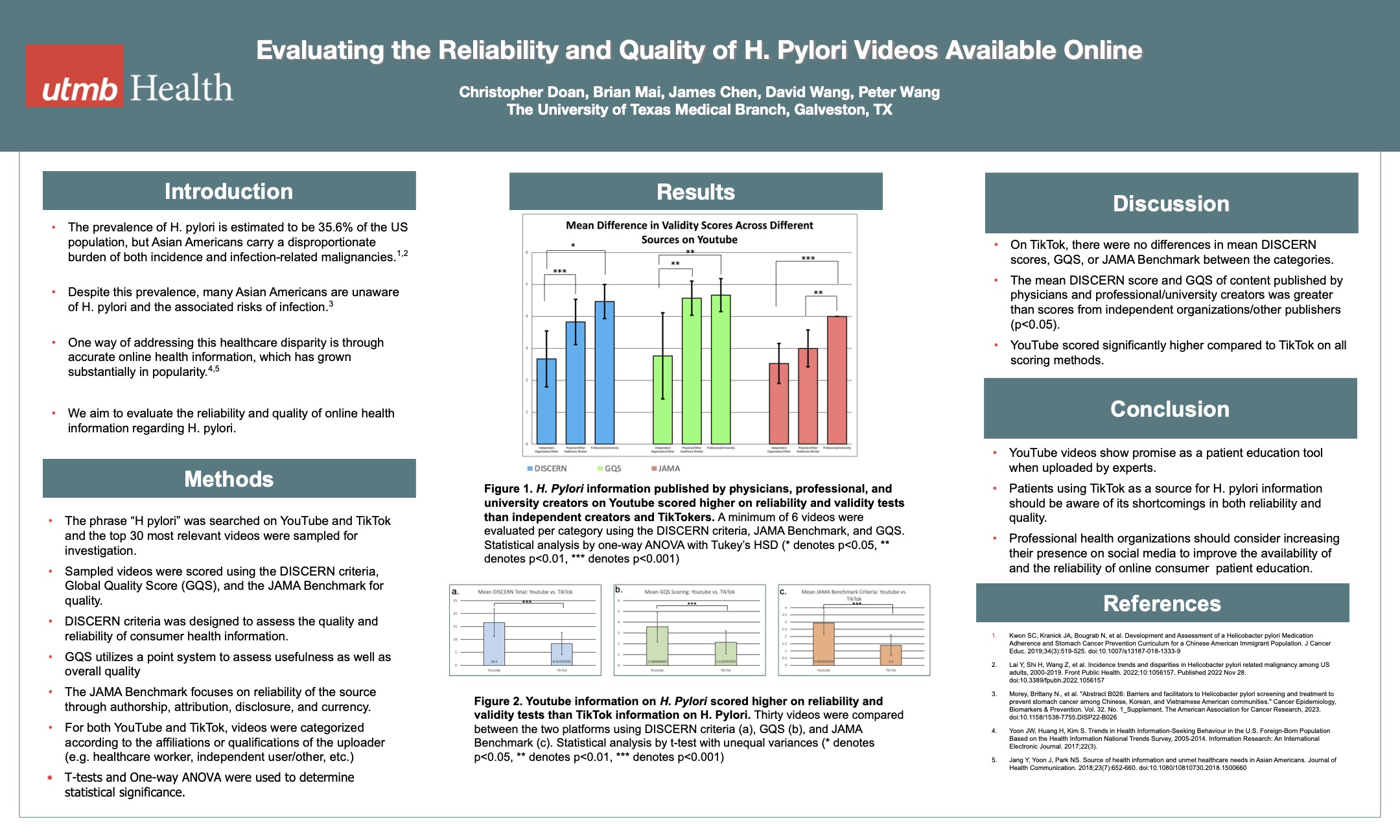
2023 National Conference Posters
Congratulations to all of our research award winners! Every year, many fantastic research projects are presented at our National Conference. Click the link below to view our 2023 National Conference Abstract Booklet, where you can learn more about the research the APAMSA community is working on.
Interested in featuring your research with APAMSA? Email research@apamsa.org for more information!
Research Award Winners
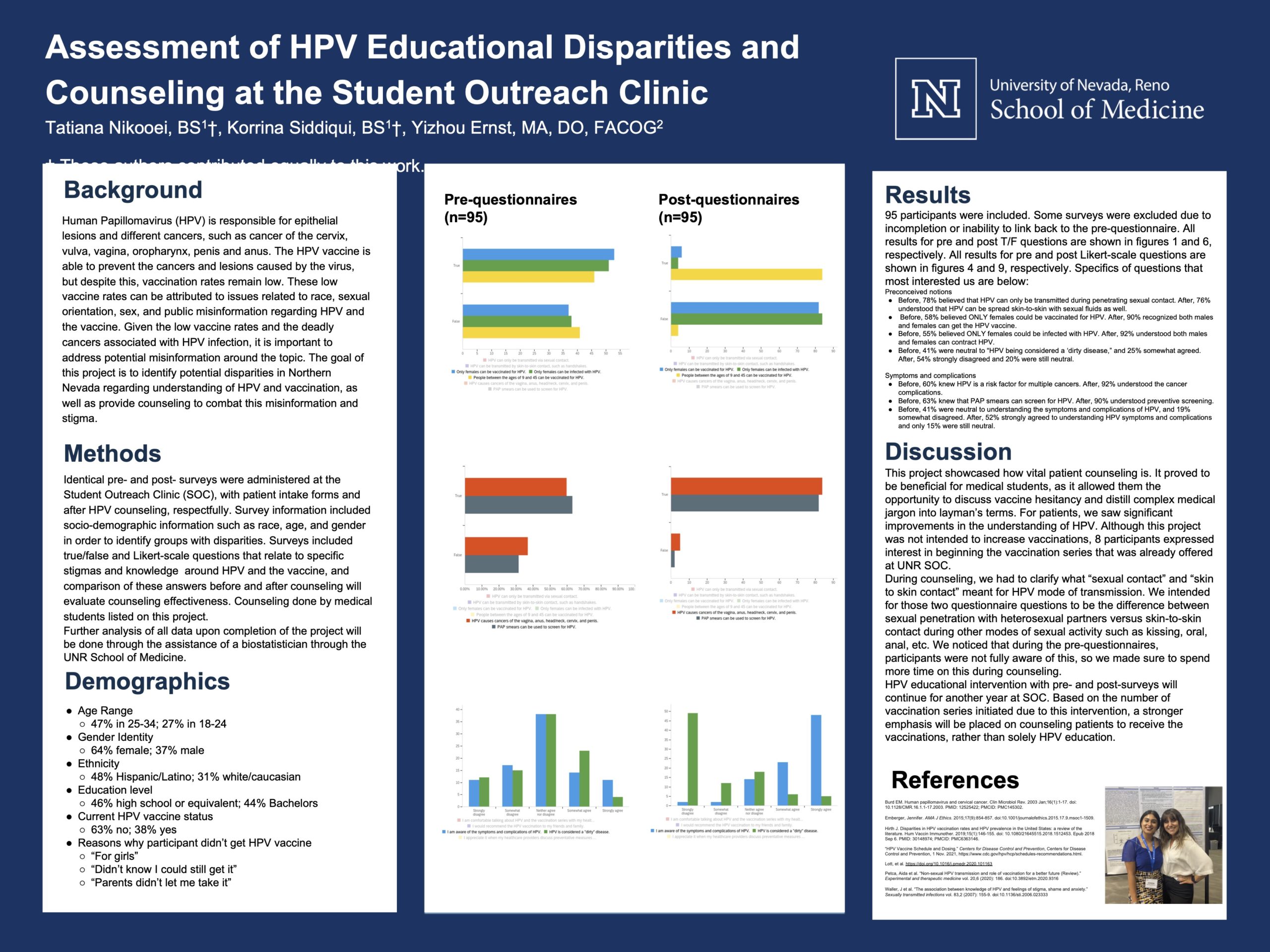
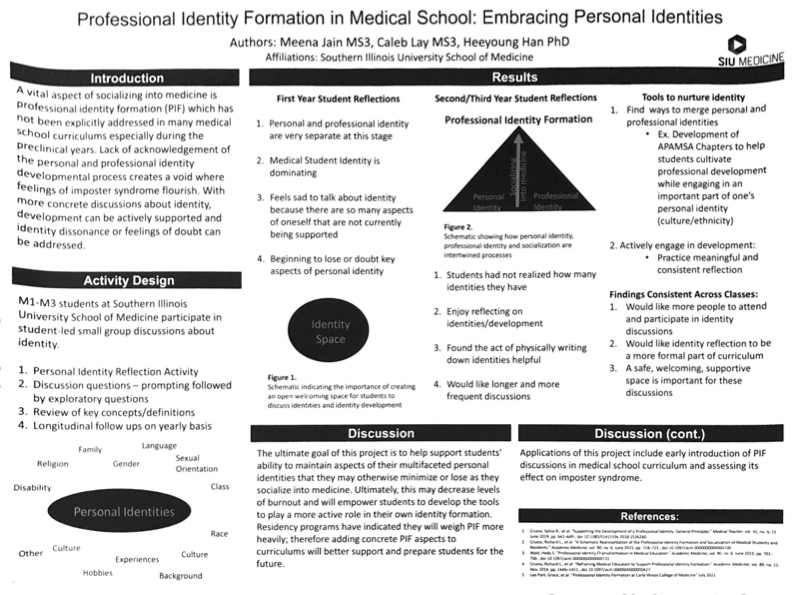
Professional Identity Formation in Medical School: Embracing Personal Identities
Presenting Author: Meena Jain
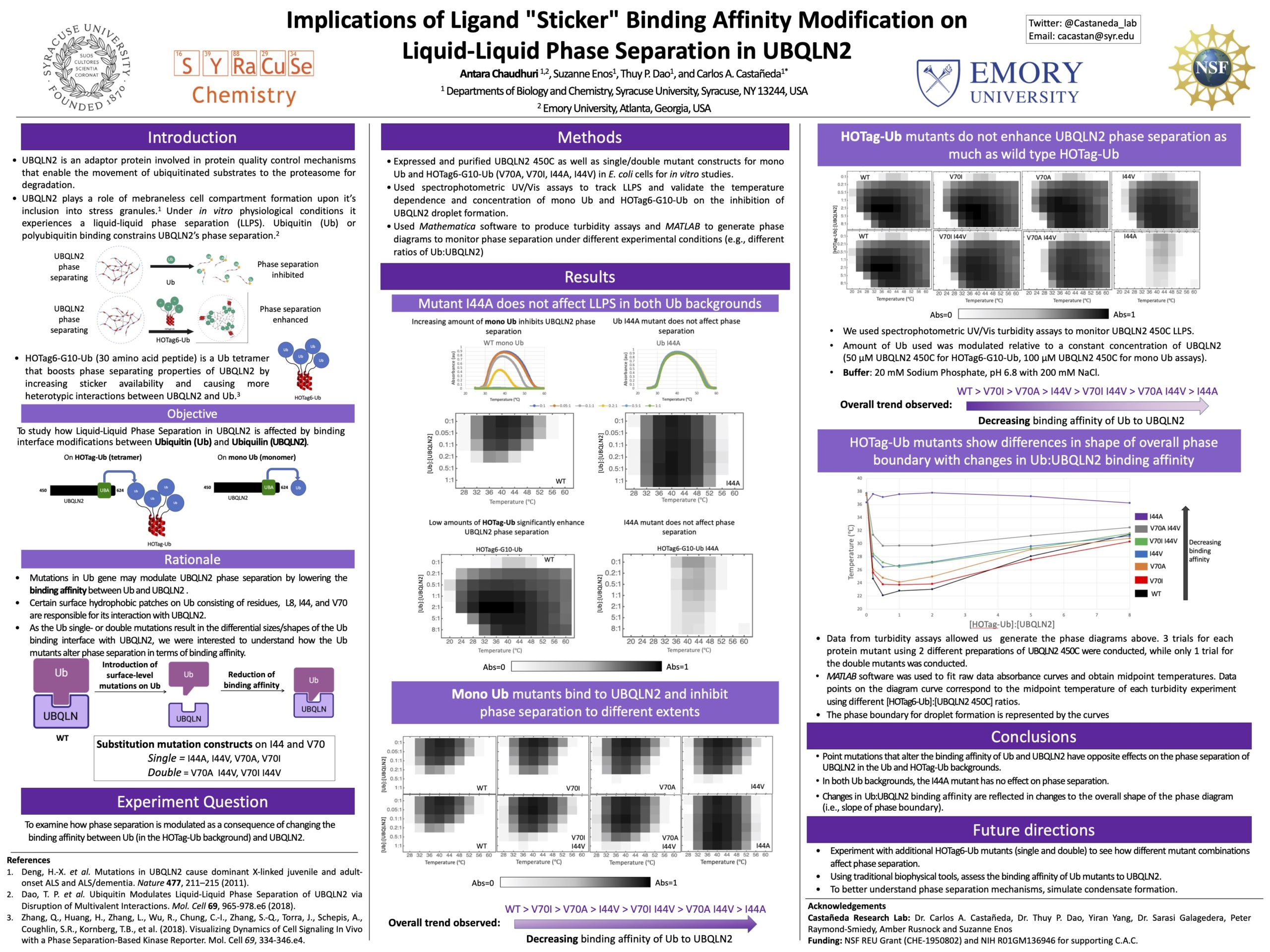
Implications of Ligand “Sticker” Binding Affinity Modification on Liquid-Liquid Phase Separation in UBQLN2
Presenting Author: Antara Chaudhuri
First Place
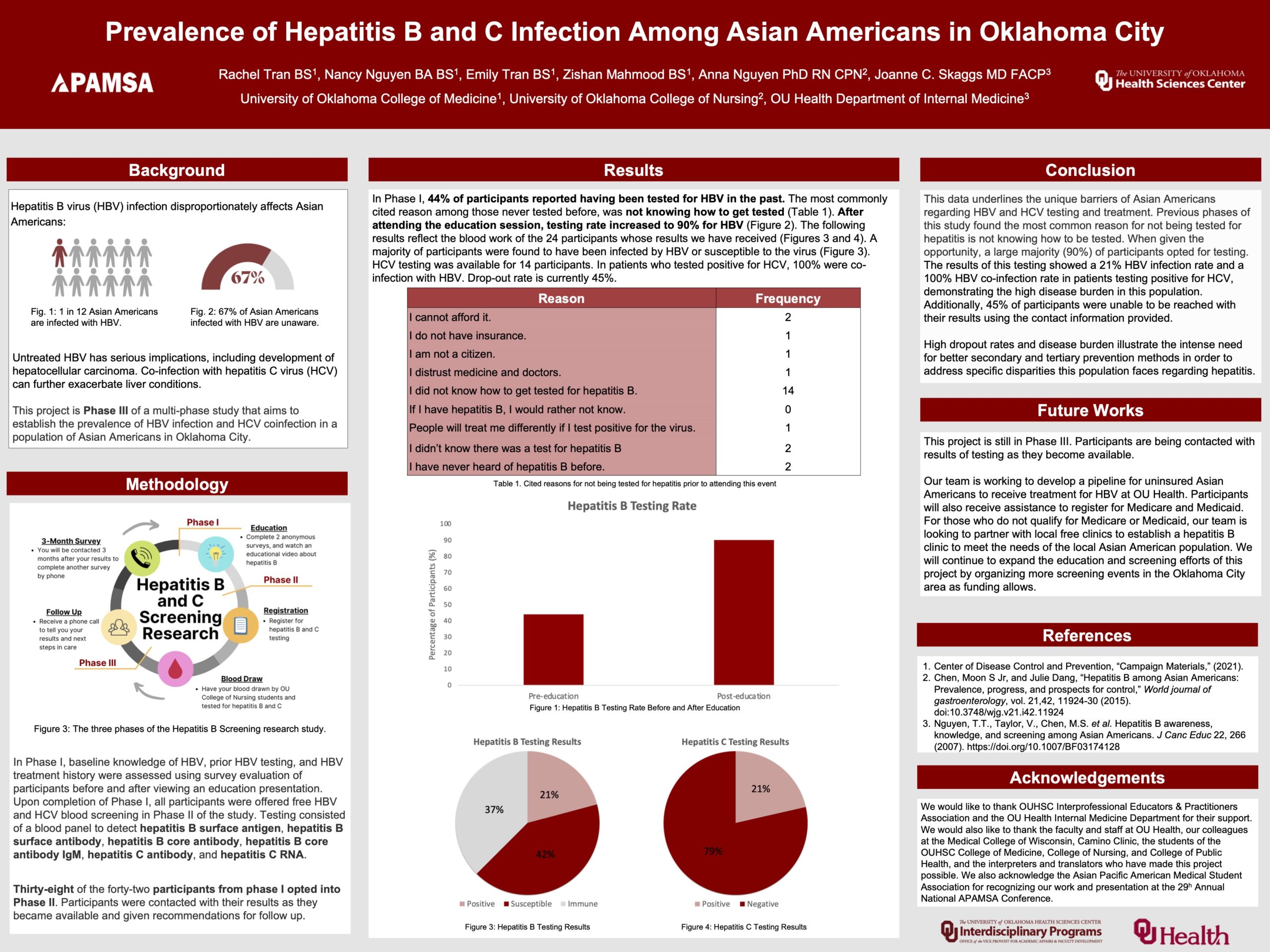
Prevalence of Hepatitis B and C Infection Among Asian Americans in Oklahoma City
Presenting Author: Emily Tran
Runner Up
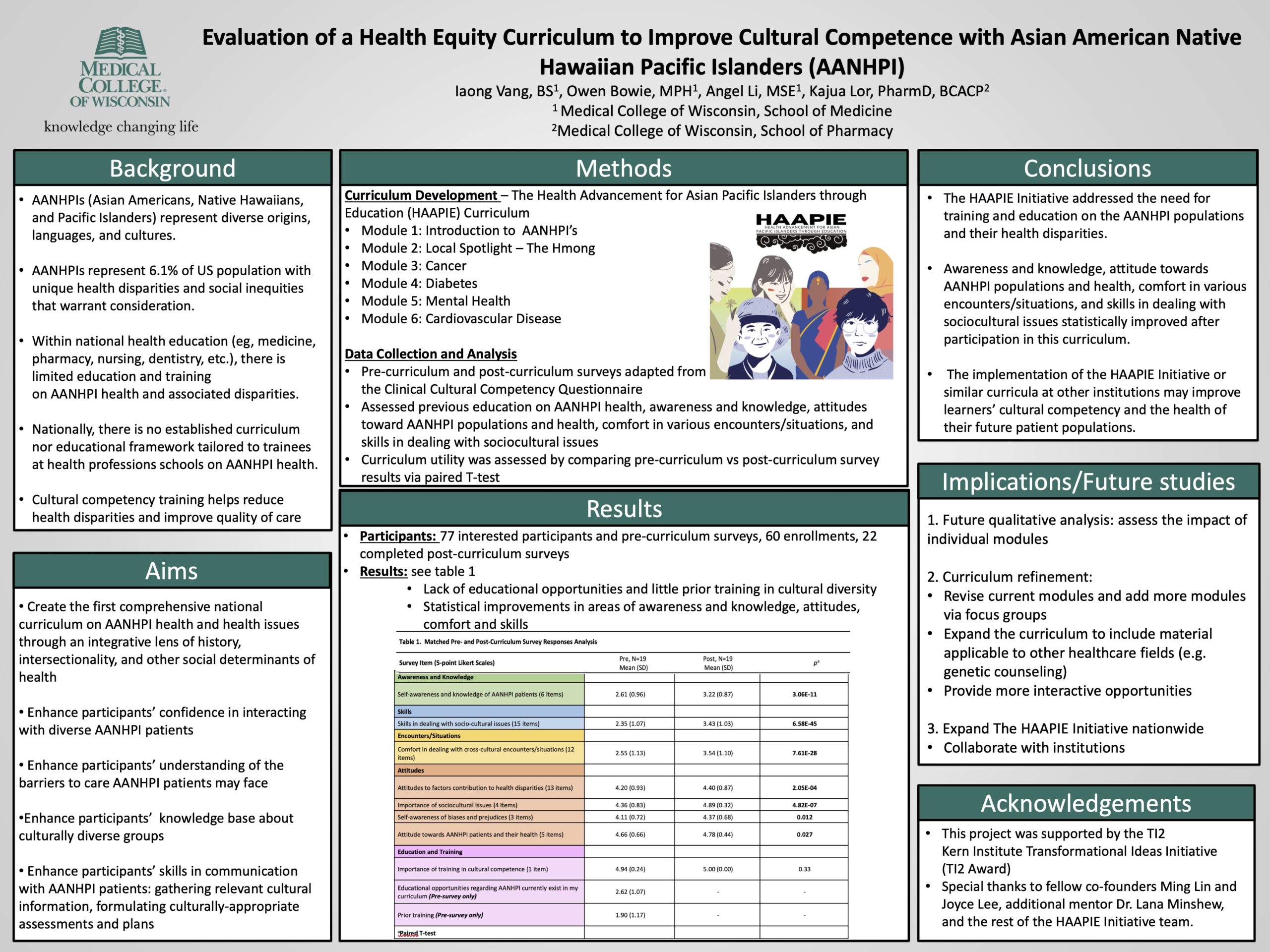
Evaluation of a Health Equity Curriculum to Improve Cultural Competence with Asian American Native Hawaiian Pacific Islanders (AANHPI)
Presenting Author: Angel Li
Runner Up
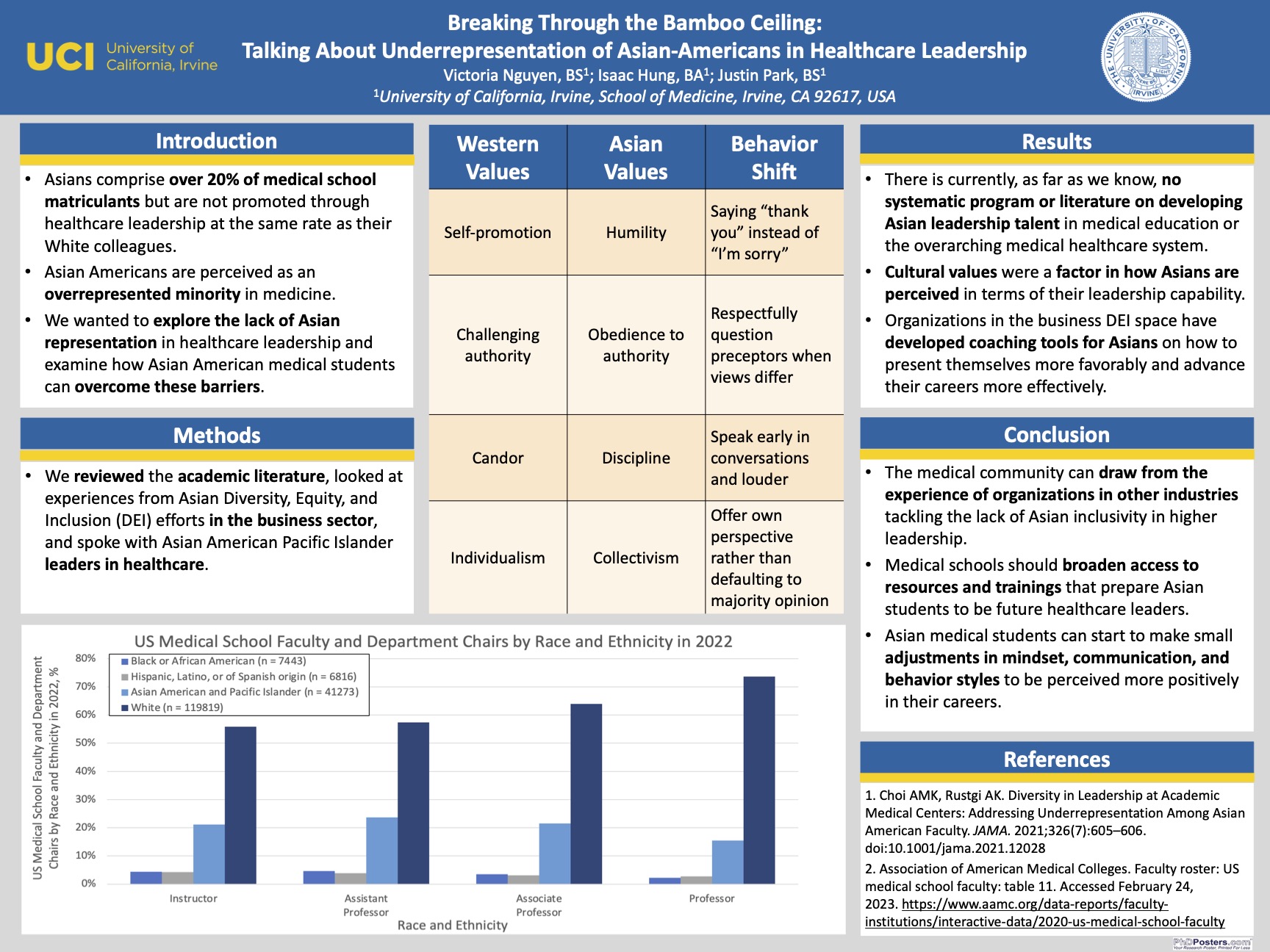
Breaking Through the Bamboo Ceiling – Talking about Underrepresentation of Asian-Americans in Healthcare Leadership
Presenting Author: Victoria Nguyen
Tori Nguyen, Premed APAMSA Co-Director
Network Director
Hello! My name is Tori Nguyen, and I am an MS2 at UCISOM. I grew up in Orange County and earned my B.S. in Biology with a minor in Global Health at UCLA. I discovered my academic interests, which include integrative medicine, hospice and palliative care, and medical education, during undergrad and my two gap years while working at a dumpling house and as a medical assistant for a gastroenterologist. I am so excited to be a Pre-Medical Director because I am passionate about mentorship and aim to promote APAMSA’s mission and service to the AANHPI community by cultivating connection within our network, creating culturally-sensitive professional development opportunities, and increasing accessibility to pre-medical resources.
LEAD with APAMSA - Building an Organization from Scratch with Dr. Jhemon Lee
Join Dr. Jhemon Lee, one of the founders of APAMSA, as he discusses the importance of leadership in the context of organizational development. He will share insights into how individuals can begin to start their own organizations, holding groups together during difficult times, and the differences of organizational leadership.
Date: Wednesday, March 1
Time: 7:00 PM EST / 4:00 PM PST
Registration Link: https://forms.gle/jehsivYEbTFGLJ3a9
Dr. Lee is a private practice radiologist in Los Alamitos, CA. He was one of the original student organizers that helped lead to the formation of APAMSA in 1995, and has helped lead APAMSA’s Advisory Board ever since. He is a board member of the National Council of Asian Pacific Islander Physicians (NCAPIP). He is president of the Orange County chapter of OCA – Asian Pacific American Advocates, and has previously been involved with the National Association of Asian American Professionals (NAAAP), serving in many roles including National President, President of its Chicago chapter, and co-chair of the 2008 National Convention. He is also the Medical Advisor for the Diagnostic Medical Sonography programs at Platt College. Dr. Lee received his bachelor’s degree in Engineering Sciences at Harvard University and obtained his medical degree from the University of Maryland. He completed his residency in diagnostic radiology at the University of Chicago, where he was chief resident, and a fellowship in abdominal imaging at Brigham and Women’s Hospital/Harvard Medical School in Boston. On the side, he and his wife, Misa performed improv comedy for years with groups such as Cold Tofu, Los Angeles’ longest running API improv troupe. More recently, Jhemon has been writing and performing sketch comedy with a local API comedy group, “No MSG Added.”
National Conference VIRTUAL Option
Hello everyone!
We’re very excited to see you soon (2 weeks!!) in Portland, Oregon for the 2023 National Conference!
If you have not yet registered, there is still the opportunity to join us at the conference virtually! The registration form and eventbrite are open for virtual attendance only.
Please fill out the form AND purchase your ticket to complete your registration. The deadline to purchase your virtual-only ticket is Friday February 24, 2023 11:59PM PST.
Looking ahead to the 2024 APAMSA National Conference, if you and your chapter are interested in hosting, we would love to know! Please email externalvp@apamsa.org and look out for information soon regarding the bid to host the next APAMSA National Conference.
Excited to meet you all March 3-5th in Portland both in-person and virtually!! You can visit our conference website for more information regarding the schedule, speakers, accommodations, and ideas for what to do when you’re in town.
National Conference Directors and Team
Cultural Competency: APAMSA Speaker Event with Dr. Kamaka
Aloha!
The NHPI Committee has invited Dr. Martina Kamaka to talk about cultural competency, the importance of culturally-relevant and sensitive care in NHPI communities, and her amazing national efforts in DEI as the AAFP DEI-FM commissioner.
Please join us on Zoom on Sunday, February 26 at 4 pm EST.
Zoom registration link: https://atsu.zoom.us/meeting/register/tJEoc-upqj4qGtDcrdEI3vniOioOKfFF6knX
After registering, you will receive a confirmation email containing information about joining the meeting.
Dr. Martina Leialoha Kamaka is a board certified Native Hawaiian Family Physician and Associate Professor in the Department of Native Hawaiian Health at the University of Hawai`i at Mānoa, John A. Burns School of Medicine. She is a graduate of the Kamehameha Schools, the University of Notre Dame and the John A. Burns School of Medicine (JABSOM). She completed her Family Medicine residency in Lancaster, Pennsylvania. Dr. Kamaka was in private practice in Lancaster, Pennsylvania and Kailua, Hawaii before joining the medical school faculty in 1999. Her passion for understanding the role of culture in medical care and wellness began during her residency training but it was as a faculty member at JABSOM that she was able to pursue that passion fully and help to formalize cultural competency training for medical students. Her passion for indigenous health has led her to current leadership positions. She is a Vice Chair of NCAPIP (the National Council of Asian Pacific Islander Physicians), commissioner for the AAFP DEI-FM commission as well as founder, past President/Chair and board member of both the ʻAhahui o nā Kauka (Association of Native Hawaiian Physicians) and the Pacific Region Indigenous Doctors Congress (PRIDoC).
We hope to see you there!
LEAD with APAMSA - Leveraging Social Media with Dr. Joyce Park and Dr. Joy Wu

The ever changing social media platforms are opportunities for prepared leaders to increase the scopes of their voices.
Join guest speakers Dr. Joy Wu and Dr. Joyce Park as they discuss how they incorporate social media into their own practices and share tips and tricks on how to get started.
Date: Wednesday, February 22nd
Time: 7:00 PM EST / 4:00 PM PST
Link: https://forms.gle/swUF2EaCjwBJuQvQ7
Dr. Joyce Park is a board-certified dermatologist based in Washington, founder and CEO of Skin Refinery, a virtual dermatology clinic, and a skincare and beauty content creator at Tea with MD. She attended college and medical school at Stanford University, and completed her dermatology residency at NYU. During medical school, she completed the Stanford-NBC News Global Health Media Fellowship, working in the communications office of the World Health Organization in Switzerland and as part of the medical unit at NBC News. She realized the power of traditional and social media for public health education during this year, and she continued exploring this potential as a fellow interning at the ABC News Medical Unit. Dr. Park created Tea With MD and its associated social media channels (Instagram, Tiktok, YouTube, and more) as a resource for science-based skincare from a dermatologist’s perspective. She strives to educate and entertain her audience of over 680k followers worldwide with a range of topics including scientific research on skincare and dermatology conditions, reviews of beauty trends, and sharing behind the scenes of life as a physician Mom. She is a skincare media expert and has been featured in has been featured in Forbes, Good Morning America, Allure, Cosmopolitan, Vogue, Huffington Post, Time, Marie Claire, the Gloss Angeles Podcast, and more. In her spare time, she enjoys exploring the beautiful Pacific Northwest with her husband and toddler son, taking hip-hop dance lessons, and mentoring the next generation of students interested in medicine and dermatology.
Dr. Joy Wu is Chief of the Division of Endocrinology, Gerontology and Metabolism and Vice Chair of Basic and Translational Science in the Department of Medicine at Stanford University School of Medicine. She earned her MD and PhD degrees from Duke University School of Medicine and completed her residency in Internal Medicine at Brigham and Women’s Hospital and clinical fellowship in Endocrinology at Massachusetts General Hospital. Dr. Wu directs a basic and translational research program that focuses on skeletal development, the bone marrow hematopoietic and metastatic niche, and stem cell therapies for bone. Her research has been funded by the National Institutes of Health, the Mary Kay Foundation and the Department of Defense. Dr. Wu has served on clinical guideline committees for the American Society of Clinical Oncology, the Endocrine Society, and the American Society for Transplantation and Cellular Therapy. She has been awarded the NIH Director’s New Innovator Award and the Stanford University Faculty Women’s Forum Allyship Award. Dr. Wu has served on the Board of Directors for the Endocrine Society and she is currently a member of the Council of the American Society for Bone and Mineral Research
LEAD with APAMSA - Communication with Dr. Judy Tung

Join our session on communication as Dr. Judy Tung shares tips on how to communicate effectively, giving feedback, and the importance of narratives.
Date: February 15th, 7:00 PM EST / 4:00 PM PST
Registration Link: https://forms.gle/bYmPfLwAPGiHVSA76
Judy Tung, MD is an Associate Professor of Clinical Medicine at the New York Presbyterian Hospital-Weill Cornell Medicine in New York City. She is a primary care general internist and is the Chief of the Section of Adult Internal Medicine in the Division of General Internal Medicine. She is also the Associate Dean for Faculty Development and directs a college-wide faculty development course called the Leadership in Academic Medicine Program (LAMP).
Best, APAMSA National Leadership Committee