Joint Statement on H.R. 1 by APAMSA, SNMA, LMSA, AMSA, SOMA, and MSDCI
On May 22, 2025, the House of Representatives passed H.R. 1 One Big Beautiful Bill Act, which contained disconcerting provisions aimed at cutting Medicaid funding by almost $700 billion over the next decade. Medicaid has been a central fixture for 83 million Americans, providing essential healthcare and long-term care for children, seniors, people with disabilities, and low-income adults. The Affordable Care Act’s Medicaid expansion to adults who earn up to 138% of the federal poverty level ($21,597 for a single adult) has insured millions of Americans with health coverage. These potential changes will deprive over 10 million Americans from healthcare coverage through Medicaid and disproportionately affect communities of color.
Medicaid has been linked to increased access in rural and disadvantaged areas and improved health outcomes like decreasing all-cause mortality by almost 2% and lowering maternal mortality. In a recent report authored by the Asian & Pacific Islander American Health Forum, the National Association for the Advancement of Colored People, the Leadership Conference on Civil and Human Rights and other national health organizations, Medicaid is the primary source of healthcare for almost 30% of people of color.
Medicaid has consistently enjoyed broad bipartisan support. A recent poll demonstrates that most Americans—Democrats, Republicans, and independents alike—favor maintaining and increasing spending on Medicaid access. Forty states across the political spectrum have opted into Medicaid expansion, recognizing the program’s role in improving health outcomes, supporting rural hospitals, and reducing uncompensated care. Despite the overwhelming evidence that Medicaid is extremely popular across the political spectrum and saves lives, House Republicans have moved to sacrifice public health in favor of funding tax cuts that primarily benefit the wealthy. The harmful provisions in H.R. 1 stand in contrast to the values shared by voters of all political backgrounds who believe Americans should not be denied care due to their income.
The bill will attempt to cut costs by
- Reducing the incentives and federal subsidies given to states for expanding Medicaid, specifically punishing any state that provides any health benefits or assistance to undocumented immigrants with lower expansion matches,
- Establish cost-sharing and copays of $35 for services provided to anyone above the federal poverty level ($15,650 for a single adult),
- Instituting stringent work requirements and eligibility verifications that burdens Medicaid recipients and state governments with more paperwork,
- Prohibiting Medicaid payment to nonprofits and providers that focus on reproductive health, family planning, and abortion services like Planned Parenthood,
- Removing gender affirming care as an Essential Health Benefit under the Affordable Care Act and prohibiting coverage for any Medicaid/CHIP recipient,
- Suspending rules that streamline application and enrollment into Medicaid and for patients who qualify for the Medicare Savings Program (covers Medicare premiums and cost-sharing for low-income Medicare beneficiaries).
We strongly condemn any legislation aimed at limiting equitable access to Medicaid or attacking access to abortion services and gender affirming care. Among the many destructive changes also embedded in H.R. 1, the elimination of federal student loans and loan forgiveness programs will severely limit access for students from all backgrounds to pursue careers in medicine. This bill proposes a lifetime cap of $150,000 for federal graduate student borrowing, specifically for those enrolled in professional programs. This will potentially force students to rely on private loans with less favorable terms and fewer protections, undoubtedly compounding the physician shortages in the very communities that rely on us.
At the heart of these proposed cuts lies an uncomfortable truth – healthcare is not a human right if equal access is not afforded to everyone regardless of socioeconomic class and immigration status. These actions go against the principles set by other nations, the World Health Organization, and the EU among others, highlighting the precarious path that the U.S. government is currently steering the country down. If passed in the Senate as is, the “One Big Beautiful Bill” will greatly harm patients across the United States and hamper the ability for physicians and other healthcare providers to serve their communities.
Call to Action:
To Senators – We call on all senators to reject this bill to protect the American public’s interest and maintain our great nation’s founding principles of “Life, Liberty and the pursuit of happiness”
To Medical Students – we urge all medical students to contact their Senators in Congress and demand a No vote on the “One Big Beautiful Bill.”
Signed,
Asian Pacific American Medical Student Association (APAMSA)
Student National Medical Association (SNMA)
Latino Medical Student Association (LMSA)
American Medical Student Association (AMSA)
Student Osteopathic Medical Association (SOMA)
Medical Students with Disabilities and Chronic Illness (MSDCI)
Additional Resources:
Contact your Congressional Representatives: https://www.congress.gov/contact-us
More information about federal student loans changes: Official Statement and infographic
Call or email your Representative today with a call script from our partner organization, Vot-ER: https://go.vot-er.org/0mAQQu
For questions regarding this statement, please contact:
Rapid Response Director, Brian Leung at rapidresponse@apamsa.org
Win a Personalized, Signed Book by Ocean Vuong!
Enter to win a personalized, signed book from Ocean Vuong (unlimited entries!) to raise money for the LGBTQIA+ Scholarship for AANHPI Medical Students!
Three books, donated graciously by Ocean Vuong and his team, are being raffled off: On Earth We’re Briefly Gorgeous, Time is a Mother, and his brand new book The Emperor of Gladness!
Click here to enter!
For questions, please contact our LGBTQIA+ Director, Joey Hua-Phan (he/they), at lgbtqia@apamsa.org
Skin Cancer Screening Toolkit

Checklist and Links to Helpful Resources
- Review Skin Cancer Screening Protocol (also linked and described below)
- Skin Screening Training Guide
- Release Form Example
- Patient Health Information Form
- Event Sign-Up Template
- Materials List
- Community Member Demographic Collection
- Additional Resources and Links
Screening Skin Cancer Protocol
For a PDF view of the protocol below, please see this link: https://tinyurl.com/APAMSASkinCancerProtocol
At least 6 months before:
- Identify a community partner. This can include any institution, community cancer center, community health center, or municipal center that is willing to collaborate with you on your event.
- Identify physician mentors. Note that this is absolutely imperative for the success of your program. You must have a licensed physician participating at the event to sign off on screening results.
- Feel free to reach out to physicians outside of your institution. Working with community partners is strongly encouraged.
At least 5-6 months before:
- Research follow-up care options and referrals to the necessary practitioners as needed.
- Secure event location, obtain funding, gather educational materials, and print necessary health forms.
- Stay tuned for the release of our APAMSA Cancer Screening Grant to aid with funding.
At least 2 months before:
- Promote your screening in local newspapers, grocery stores, churches, and other areas in your community.
- Have online sign-up forms prepared and advertised so that clients can schedule an appointment.
- Start gathering all necessary materials (PPE, gowns, penlights, etc.).
At least 2 weeks before:
- Recruit and train volunteers – roles may include navigators, room turnovers, and desk clerks at check-in/check-out stations.
- Determine volunteer schedule. Go over protocol with them.
Day of screening:
- Volunteers hand out educational materials, register clients, and collect the proper forms (release forms, health info, self addressed envelopes).
2-3 weeks later:
- Contact everyone who participated in the screening via letters or phone calls regarding their screening results.
- Follow up with community partners and debrief on the event.
- Complete and submit Event Feedback Report to the APAMSA Cancer Initiatives Director.
Please contact cancer@apamsa.org in advance if you will be organizing a screening program and would like to participate in the national APAMSA effort to increase community access to cancer screening and education.
A full list of links to find healthcare access aid resources in your local area along with multi-language materials to utilize at your event can be found here.
Step-by-step protocol:
- Identify your population or community of focus. We highly recommend reaching out to local community organizations to discuss partnership.
- Identify a local physician (primary care, dermatologist, oncologist) who will serve as your mentor and oversee the screening.
- Important point: It is absolutely imperative you work with a physician for your program. Reports given to screened subjects must be signed by a physician.
- The American Cancer Society offers a list of databases to help allocate physicians in your area.
- Determine the cancer outreach and language needs in your area. Refer to this collection of multi-language cancer awareness pamphlets for examples of resources.
- Note: It is important to implement resources and an action plan that are inclusive of diverse skin tones and colors.
- Identify materials needed for the screening: Feel free to refer to this Materials List as a guide. Quantity and costs are subject to change.
- Secure funding to cover the cost of materials. APAMSA is setting up a Cancer Screening Grant application, so stay tuned for opportunities to gain funding.
- Research the following questions.
- Where can insured screening-positive clients obtain care?
- Provide referral information for physicians who see clients with suspicious skin lesions. The client’s own PCP is also sufficient.
- Where can uninsured screening-positive people obtain care?
- Provide information regarding clinics for the uninsured – find community health locations using this link.
- Are interpreters needed for your event?
- You may need to seek peer educators or AANHPI advocacy groups to recruit multi-lingual volunteers to serve as patient navigators, since many community health clinics do not have resources for interpreters for many Asian languages.
- Refer to the Additional Resources document for interpreter resources if needed.
- Where can insured screening-positive clients obtain care?
- Develop a client follow-up plan
- How will you ensure that clients who need further follow-up are able to contact any referrals made?
- E.g. additional phone calls to make sure the clients have contacted a primary care provider or have made an appointment.
- How will you ensure that clients who need further follow-up are able to contact any referrals made?
- Identify an appropriate screening location.
- This can be at a clinic that sees Asian patients, a cancer institute, a church, community center, or your local campus. For your screening event to go smoothly and efficiently, it is recommended that your venue has a waiting area, an area for check-in, at least two or more private rooms with seating, an area for check-out, and plenty of hallway space for multiple people to walk through.
- Obtain educational materials in English and Asian languages regarding skin cancer to distribute to the clients who come to your screening. Use existing materials from the CDC, American Cancer Society, The Skin Cancer Foundation, the American Academy of Dermatology, etc.
- Refer to this collection of multilanguage cancer awareness pamphlets for examples of resources.
- Print and organize all necessary forms: Our cancer screening toolkit contains examples of release forms and patient health info forms that you may utilize.
- If applicable, consider the need for translated versions of these forms based on the population you serve.
- Recruit and train volunteers; these may be students or members of community partner organizations. For a screening event that lasts multiple hours, you may assign hourly shifts to volunteers.
- These volunteers will be responsible for turning over rooms, serving as navigators, working at check-in and check-out stations, and some may participate in performing skin exams with a physician’s oversight. Assign a lead volunteer to be in charge of rooming and collecting forms.
- Advertise your event to members of the local community. Create registration forms that request contact information of clients who are scheduling an appointment. You may also request contact information of the client’s primary care provider (if applicable) to send results directly to them after your screening event. Distribute fliers to communal areas like grocery stores, churches, or recreational centers. See examples of fliers provided in our toolkit.
- Send out a reminder to all registered participants a week to a couple days in advance of their appointment time and event location.
-
- Have student volunteers ready at different stations.
- a. Check-in: Have clients fill out a health info form and a release form – see examples in our toolkit. Inform the client to take these two forms with them to the exam room. Keep an organized log of every client, their appointment times, and contact information to keep track of all clients who present to the screening. Have seating, clipboards, and pens available for those who are filling forms or are waiting to be seen.
- b. Screening Station: Each room should be turned over and prepped for every new client to be seen. A complete room should have all necessary PPE (gloves, masks, hand sanitizers), measuring tape for recording suspicious lesions, a clipboard and pen for the examiner, and a fresh gown for the client. Make sure each client is given plenty of time to change before being seen by an examiner.
- Use colored indicators on doors to track the status of each room: (1)vacant and ready for a new client, (2)occupied with a client who has yet to be seen, (3)occupied with both client and examiner, (4)vacant but needs to be turned over. You can use a binder ring with four different colored construction papers placed on a hook or doorknob.
- You should assign a volunteer as a lead who is in charge of rooming. This person assigns clients to vacant rooms and allocates an examiner to each client who needs to be seen. After each visit is complete, the lead should collect all Release forms from the client, and direct the client to a navigator to be escorted to check-out. The client should have only their Patient Info Form with them at check out.
- You should assign additional volunteers as navigator or room turnovers. Navigators are to escort clients from check-in to their screening station and back to check-out. Navigators should also double check that all client forms are handed to the lead. Room turnovers are to keep all rooms stocked with supplies and prepare a new gown for each client.
- Have student volunteers ready at different stations.
- Check-out: It should be recorded when each client has finished their screening and left the facility. Make sure to scan a photocopy of each client’s Health Info Form; they can take the physical copy with them for their own records or if they choose to present it to their provider at a follow up visit. At this point, volunteers can double check with the client that their logged contact information is correct in case you would like to follow up with them. Also confirm with the client that their PCP information is correct, or if they require referrals based on their insured status. Inform the client that their screening results will be sent to their established provider if they have one.
Overview of Screening Responsibilities:
- Positive for a suspicious lesion
-
-
- Recommendation: further testing, referral to a primary care physician, or follow-up at a clinic that accepts uninsured clients.
- For insured clients:
- Identify a physician/physicians in your area who specialize in skin cancer (dermatologists). Refer clients to these physicians, or encourage them to make follow-up appointments with their own primary provider.
- For uninsured clients:
- Ideally, identify and refer clients to a community health center dedicated to the Asian population.
- If unavailable, refer to a community health center, a clinic for the uninsured that provides Asian language services, an established navigator system, or a student run free clinic affiliated with your institution. Be aware of what referral systems and services are offered at your student run clinic.
- For insured clients:
- Recommendation: further testing, referral to a primary care physician, or follow-up at a clinic that accepts uninsured clients.
-
- Negative for suspicious lesions
- Recommendation: Encourage education and promote awareness.
-
-
- Educate clients that a negative screening result does not eliminate the possibility of skin cancer. Inform them of risk factors and prevention methods. Emphasizing sunscreen use is crucial. They should also be encouraged to perform self-examinations at home to identify any new or changing skin lesions which they can bring up to their primary care physician.
-
Client Follow-up Protocol:
- All clients with an established primary care physician should have their Health Info Form sent over to their provider’s office.
- It is ideal to follow up with everyone who participates in your screening to educate them about skin cancer and direct them to appropriate avenues for treatment.
- Important point: simply telling clients at your screening event to go see their primary care physician is not as effective as calling and writing to them directly.
- With direct communication, we can ensure that 1) clients understand what they need to do, and 2) they understand the reasons for doing so.
Examples of Client Follow-up Systems:
- Letters
- If you send out letters to your clients, make sure they are in English and appropriate Asian languages.
- Ensure that the language you use is readable and accessible to people with all levels of literacy. Avoid unnecessary jargon.
- Make sure your letters are customized with information regarding clinics, referrals, and skin cancer info.
- TIP: When you register people for the cancer screening, have them self-address an envelope to themselves that you will use to send them their results. This will minimize mistakes in mailing addresses.
- Letters and Phone calls
- Sending letters and following up with phone calls is a better way of making sure the people understand their screening results.
- Make sure that if you make phone calls you have people who can speak the language of the person you’re calling, either through recruiting volunteers who speak other languages or using phone interpreter services.
- If you mail a letter, try to follow up with a phone call 2 weeks later to make sure they understand the letter and encourage follow-up. Then, make a follow-up call 3 months later to see if action was taken. The downside to making phone calls is that you can’t give medical information to anyone except for the person you screened, so you may have to call back several times.
Handling Patient Info:
- You should keep all physical copies of signed Release Forms on file for proof of HIPAA compliance. Any client is allowed to request a copy of their Release Form.
- All clients should leave the event with the physical copy of their Health Info Form after you scan a photocopy and store it digitally in a private location. Ensure that only your institution, club executive board, and/or partnered organization’s administrative members have access to these documents. You may send copies of Health Info Forms to your clients’ primary care physicians with each client’s permission.
- Make sure to discard all physical copies of sensitive documents appropriately if they are no longer needed (i.e. by paper shredding).
It is recommended before you proceed with anything to talk to your schools and partnered organizations regarding the best way to handle this.
While there is very little risk involved with skin cancer screening, every institution and health organization has different policies which you must understand before proceeding with any service that informs patient care. This is another reason why the first and most important step is to secure a licensed faculty/ physician advisor to oversee your screening.
We’d love to hear about your experience using this toolkit! If you have any thoughts you’d like to share regarding what we’ve done well and where we can improve, please fill out this feedback form.
Intersecting Narratives: Exploring Generational Differences in Maternal Health Factors in Vietnamese Mothers of Children with Orofacial Clefts
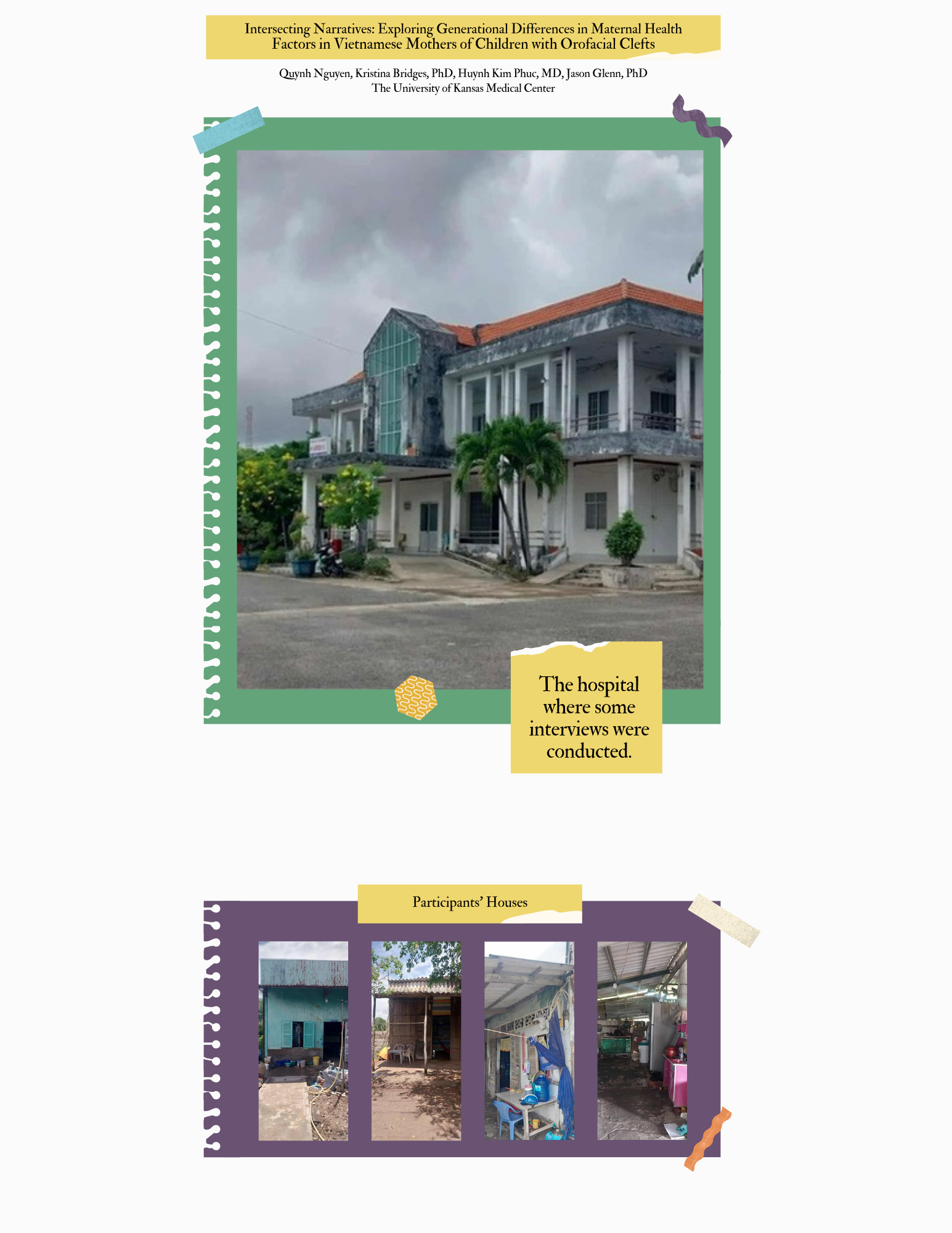
Clefts Without Borders
The voices of the women I interviewed will stay with me for a long time. They’ve reshaped how I think about healthcare, equity, and the role of a physician. And they’ve deepened my commitment to becoming not just a doctor, but a better listener, advocate, and bridge between cultures.
Quynh Nguyen, MS3 at The University of Kansas Medical Center
Women in Medicine Conversations: KAN-WIN

KAN-WIN is a culturally specific nonprofit organization based in the Chicago area that serves Asian immigrant and Asian American survivors of gender-based violence. In this Women in Medicine Series episode, Abbey Zhu from KAN-WIN discusses the services KAN-WIN provides, challenges that AANHPI survivors of violence face, and how health care providers can learn and provide trauma-informed care for their patients.
Listen here:
YouTube
Spotify
Apple Podcasts
This episode was produced by Anne Nguyen, Eujung Park, and Ashley Tam, hosted by Anne Nguyen, and graphic by Callista Wu and Claire Sun.
Time Stamps:
00:00 Introduction to Women in Medicine Conversations: Abbey Zhu from KAN-WIN
00:55 Introduction to Abbey Zhu and KAN-WIN
02:21 Unique Challenges for AANHPI Survivors of Violence When Seeking Support
06:11 How to Start Conversations with the Community
11:32 Creating a Safe Space for Patients
15:18 Recommended Trainings to Learn Trauma-Informed Care
17:55 Misconceptions About Trauma and Its Impact On Patients’ Health
21:19 Policies to Improve Trauma-Informed Care
24:42 How to Connect with KAN-WIN
25:47 Wrap Up
Full Transcript:
00:00 Introduction to Women in Medicine Conversations: Abbey Zhu from KAN-WIN
Anne: Welcome everyone to a new episode of the Asian Pacific American Medical Student Association Podcast. From roundtable discussions of current health topics to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization, this is White Coats and Rice. My name is Anne Nguyen and I am the Women in Medicine Director at APAMSA. I’ll be your host for today. Today we’ll be meeting with Abbey Zhu from KAN-WIN as part of our Women in Medicine Series in the APAMSA Podcast. In this podcast, we dive into topics ranging from experiences as an Asian American Native Hawaiian Pacific Islander (AANHPI) woman in medicine, to broader topics like women’s health advocacy. Abby will be sharing with us today about KAN-WIN’s mission and their work in working with domestic violence survivors and other survivors of violence within the AANHPI community.
00:55 Introduction to Abbey Zhu and KAN-WIN
Anne: Hey everyone. So we’re here today with Abbey from KAN-WIN. Abby, could you go ahead and introduce yourself first and a little bit about KAN-WIN?
Abbey: Yes. Hello, my name is Abbey. My pronouns are she/they and I’m the community engagement team lead at KAN-WIN. And KAN-WIN is a culturally specific nonprofit organization based in the Chicagoland area, serving Asian immigrant and Asian American survivors of gender-based violence. So what that looks like is we serve survivors of domestic violence, dating violence, sexual violence, and we have direct services available for them. So that includes legal advocacy, counseling, general wraparound case management, but we also have a super robust community engagement and outreach and education team. So we’re doing both the immediate crisis intervention work, but also trying to lay the foundations for a lot of community and social change so that hopefully we can equip all community members,
regardless of whether or not they’re working for a domestic violence agency with the skills, knowledge, and confidence to be able to support and advocate with survivors of domestic violence.
Anne: Thank you for sharing about KAN-WIN’s mission. It sounds like you all do a lot of great work within the community, especially with different multifaceted approaches, like you were saying.
02:21 Unique Challenges for AANHPI Survivors of Violence When Seeking Support
Anne: I was wondering if you could share with us some unique challenges that Asian American, Native Hawaiian Pacific Islander survivors of trauma and violence face when seeking medical or psychological support, especially because KAN-WIN has such a strong, culturally responsive focus.
Abbey: Yeah, I forgot to mention this during the intro, but at KAN-WIN, our staff speak Korean, Mongolian, and Mandarin Chinese, and we were actually founded by Korean Advocates in 1990. So this is our 35th year anniversary of serving clients in the Chicagoland area. But related to that, right, because we’re doing both the direct service work and doing the community outreach and education work, just getting a general pulse on how the community’s doing, kind of what victim-blaming attitudes they might be internalizing, and then also just the fears that survivors themselves might face in like coming forward, asking us for help, even identifying as a survivor. I think especially in a lot of immigrant communities, a lot of our communities are very tight-knit, right? We depend a lot on each other because obviously the United States is not an incredibly welcoming space for immigrants, an incredibly welcoming space for people of color. It’s so beautiful, the ways that we’re able to build these strong communities, but at the same time, because of how tight-knit they might be, there’s a really strong fear of gossip, or there might be a really strong fear of folks stepping, “stepping out of line,” and so there might be a lot of silencing or shame in identifying as a survivor of domestic violence. I think one of the most prominent issues that KAN-WIN has been addressing since our founding is even identifying or naming something as violence. When people immigrate to the US, after they get to the US, there’s so much structural, systemic, and also interpersonal violence that people might feel like they have to normalize or be okay with to literally just survive. So I think the biggest challenge is what someone might perceive as normal, actually naming it as violence and being like, “This isn’t okay.” And I think for a lot of people, too, they might have grown up in families where there wasn’t mutual respect between parents or there might have been power dynamics between parents or power dynamic between parents and children. And when there is a power dynamic, then violence might be seen as justified, right? So I think our biggest challenge has been going out into communities, doing a lot of education around healthy relationships, not just like, “How do you identify domestic violence?” but like, “How do you actually build a healthy relationship with the person you’re dating, the person you’re married to, parents and children?” And how do we talk about things like consent not just in the terms of like sex and dating, but also between family members and trying to change the norms around how we are in relationship with each other, especially while dating or within the family, and really, really pushing for that like, norms change at the community level, not only so that we build those healthy communities and families and relationships that we want to see everywhere, but also so if someone does experience violence, that they’re able to identify it, name it, and not have any fear around disclosing to people.
Anne: Yeah. Yeah, I think that because this is such a sensitive topic, a lot of the time you want to make sure that you cultivate a safe space for that person to come forward themselves and be willing to put themselves forward in a way that, like at their own pace, everything like that.
So I think like you were saying big issues are like just starting the conversation in the first place and then getting a sense of what that person even thinks is normal or what they’re like potentially minimizing in their lives.
06:11 How to Start Conversations with the Community
Anne: I was wondering for KAN-WIN, because you were talking about education and community outreach for y’all, how do you guys get people to be receptive to your efforts, or how do you start these conversations in the first place?
Abbey: Yeah, that’s such a good question. And I think it’s something we continue to try to figure out. I mean, at KAN-WIN, we have a multilingual advocacy team as well as community engagement team. So we work together, but we’re also separate departments. You can think of us as separate but partner departments. And for our multilingual advocacy program, they are people who are bilingual, so fluent in an Asian language and also fluent in English. And they explicitly do education and outreach to immigrant communities where people might not be speaking English as their first language. So we have a Mandarin Chinese speaking advocate, a Korean speaking advocate who also does a lot of targeted outreach to Korean faith communities, so Korean Christian communities, and then we also have a Mongolian advocate.
And I think it helps so much, obviously to be able to do things in language, so much of our values are also embodied in our language and that– being able to have someone who can translate and interpret so skillfully is really important. And then also I think, depending on like what generation immigrant you might be, that also is going to change your lived experience, your values, and the way that you move through the world. So I think having that team is so, so helpful because they’re generally targeting older folks, first generation folks, people who don’t speak English as their first language, and really just laying the groundwork for, okay, like, hey, like a lot of the things that you’ve experienced in life are really, really messed up. Like, a lot of them can change and can be different, especially for future generations. And on the community engagement team, we’re mostly English speaking, we have a youth and young adult organizer who explicitly does education and outreach to Asian American high school students. We focus on college students, and then also like professional to professional training, like certification training, sexual harassment training, bystander intervention, etc. But what we’ve been trying to do is try to also do more, just like intergenerational dialogue. So actually, this past February, our youth and young adult organizer, our faith advocate, our Korean speaking faith advocate, and then also members of our direct service team did a whole month of workshops and programming with Korean churches. So they did workshops on teen dating violence because February is teen dating violence awareness month. And they did workshops just for the parents specifically, just like what they should know about teen dating violence, how to support their children, how to maybe identify as well. And then for the teens themselves, our youth and young adult organizer and an art therapist on staff did workshops around boundaries, consent, basically how to maintain healthy relationships. Think about healthy relationships, both within the context of family but also dating. And an art therapy workshop that kind of also helps facilitate, ‘How do I want to set up boundaries? What kind of boundaries do I want to enforce’, etc, etc. And they also created a brochure so that parents and children could have a dialogue with each other. And so this very targeted intergenerational outreach I think was super well received. I mean it’s something that parents will always be worried about. They don’t want their children to be facing violence right. Then for children, empowering them to be able to keep themselves safe and then also set the foundations for the types of relationships that they want to have was so, so helpful. And I think like we want to keep being able to do that into the future because I think parenting workshops have been super helpful, especially among first gen immigrants, people who don’t speak English as their first language and our multilingual advocates have done consent and parenting workshops so often. And we want to be able to keep developing that and keep creating conversations between generations, just that we can like really clearly emphasize that there are folks in the community who are thinking about this who recognize that mental health is a really big issue, that creating healthy relationships is really difficult within immigrant families. And how do we start doing that, start saying like, some of these things that might have been seen as normal are actually not okay. And how do I know that other people also have my back and are going to support me and trying to create a different or better future for all of us.
Anne: I think that you brought up really great points about like the very targeted interventions because you know, this is– these are like issues that affect many people of like many different backgrounds within the same community. I like the work that you did with the Korean communities and things like that because it’s just you’re really utilizing something that is like a sense of a support system for people who are going through things and then by partnering with them, you know, you can create a much stronger and safe space for people to talk about things.
11:32 Creating a Safe Space for Patients
Anne: I think for us as future health care providers that learning how to build and create the safe supportive space is something that we’re always keeping in mind when we talk to patients. I’m just wondering if you had any tips for how clinicians or health care providers can navigate these conversations about difficult topics like violence, especially maybe in terms of language so we can approach care without actually traumatizing or just kind of like accessing the situation when we meet patients who we think might be going through something.
Abbey: Oh, that’s such a good question. And like my first instinct to answer that question is just like to be curious about your patients to ask questions that might not just be directly related to their symptoms of where they’re coming in to seek care for, but genuinely being curious about
patients’ lives and getting the context for why this person came in, in the first place. And I think just having longer conversations with someone reveals so much, especially for domestic violence survivors or really anyone who is a survivor of like racialized violence or economic violence etc. Right? What, beyond like the medical care that can be provided, maybe I can refer someone to a social service organization that could provide economic financial assistance or housing assistance rental assistance, if someone’s worried about insurance or like paying for their health care, and giving them information about Medicaid or other affordable health care options in your city or in your state. I think with domestic violence. I’m sure I’m quite sure almost every state has their own version of what might be called “40 hour training”. And that’s basically just a really intensive training where you get trained on how to identify domestic violence, identify dynamics of domestic violence, how to support survivors, and basically also how to treat survivors in a– as much as possible trauma informed way. And I know the word trauma informed is such like an amorphous like bubbly word, like what does that actually mean? But to me it really just means recognizing and acknowledging that no one ever faces violence, whether it be domestic violence whether it be medical violence again like economic violence, racial violence etc. None of that happens in a vacuum, and like understanding on a deep level that the world that we live in is so unjust and so many different ways. And so when someone comes to me because they’ve experienced violence in some way or another, recognizing that it’s never just on the interpersonal level but there are so many reasons why that person experienced violence and why they’re here today, and like trying my best to be able to be able to understand the context in which the violence happened and not just like the manifest– maybe the physical manifestations of violence in the current moment. So I think just being curious, asking questions, and trying to get as much context as possible and then if you have the time, and you can get your workplace to pay for it because it’s usually so expensive, getting 40-hour-trained is super super helpful in just getting a deeper understanding of what domestic violence looks like and how to specifically support survivors.
Anne: Yeah, I think that, what you were saying about the training and figuring out the context it’s all so important and something that we need to keep in our minds constantly. Someone might not be coming to you to tell you their whole backstory but then if you kind of like make a space, elicit information, you can, you know, then gather that context and really help them to the fullest.
15:18 Recommended Trainings to Learn Trauma-Informed Care
Anne: I’m really interested in the 40-hour-training that you were talking about I was wondering if you could tell us more about that or other resources and training that you would recommend medical students and other clinicians within this– working with this community who want to improve their ability to provide trauma informed care.
Abbey: Yeah, so the 40 hour training is specific to Illinois. In Illinois, if you want to work with domestic violence survivors in a one-on-one setting so work at a domestic violence agency, volunteer for a hotline, volunteer for a shelter etc. So if you’re looking to get 40 hours of training first before you can start working with those survivors. Basically it’s just a law that’s like we want to make sure that folks working with survivors are not going to retraumatize survivors. In New York or in other states, yeah, quite confident that there are probably other training requirements for y’all, but generally domestic violence agencies or organizations will host 40-hour-trainings throughout the year, you can register for them. So some of them are all online some of them might be 20 hours of self paced learning 20 hours of in person training, but it is a really really great way to get really really in the weeds of just dynamics of domestic violence, legal options for survivors, medical options for survivors, and also like history of the anti-violence movement as well. So it’s really like kind of like foundational training for you to be able to expand your knowledge of how to support survivors of gender based violence, intimate partner violence.
In terms of other trainings I think really just any professional trainings that you can register for that deepen your knowledge of anti bias work, just anti racism, just any trainings where you can learn more deeply about the structures and systems of our world and how they impact people on the individual level and how that’s going to impact the way they show up when they come to a hospital or when they come to a clinic or when they come to the doctors. I think there are so many really amazing organizations who provide and do trainings on that, because, again, like we grow up in a world learning so many narratives about so many different people. And so there’s a lot of stuff for all of us to unlearn, because our brains are wired to think in very specific ways and we might not even be noticing, that we’re thinking or behaving and therefore acting in a way that is actually really harmful towards other people. So yeah, those are my recommendations.
17:55 Misconceptions About Trauma and Its Impact On Patients’ Health
Anne: On that topic, then, what do you think are some common misconceptions about trauma and how it can impact patients health and well being just so we will know to look out for what we want to unlearn and things like that.
Abbey: Yeah, I think, in the context of domestic violence, the biggest misconception is that the only thing that counts as domestic violence is physical violence, so people might only be looking for physical signs of injury, whether that be bruises like choke marks around the neck broken
or whatever. But what we know as folks working in the anti-violence movement as people serving survivors of domestic violence is that domestic violence is so much more than that. It could look like sexual violence, including sexual assault, it could look like tampering with someone’s birth control forcing someone to have a child if they don’t want to have a child, it could look like emotional abuse, psychological abuse, financial abuse, not letting someone get a job, not letting someone have their own bank account, and like that doesn’t manifest physically
right but all of that trauma, even if it is like “psychological” is going to show up in the body in different ways. So a lot of our survivors might be like, “Oh, like, I’ve had chronic stomach pain for months”, and like that’s stomach pain obviously is a manifestation of like the abuse and violence that they’ve been enduring, but it shows up as this like body problem that might feel like, “where did this come from?” and also like, oh, at the same time like “that’s just a stomach ache”, right. But as y’all know, as medical professionals, as medical students, all of the violence, even if it isn’t physical, is going to show up in our bodies in different ways, whether that’s mental health difficulties or issues, whether it’s chronic pain, chronic stress, high blood pressure, headaches right? Thinking about that and then also thinking about how you never really, “completely heal” from trauma. It’s always going to stay in the body in some way or another might show up as PTSD again, might show up as chronic pain, but just like getting rid of the idea that like, things can be “fixable”, but rather empowering survivors giving them the tools, the empathy and the space to decide for themselves what they want their healing journeys to look like. And also being really honest with survivors. I think that’s something that we repeat over and over again is that we’re never going to over promise to survivors when we do legal advocacy right? Applying for a restraining order or order of protection– when we help clients apply, we’re not going to say like, “you will be able to get this for sure” right? We’re going to be like “hey we’re going to help you get this, it’s ultimately up to a judge”. And I feel like in medical context, it’s a similar thing of like “we’re going to do our best to address this and work through this together”. But again, right like there’s no guarantee that it’s going to be over or gone completely.
Anne: And so after sharing about that I do think that, like you were saying, it’s really easy for people to get caught up with these kind of “classic or typical expectations” of what like a survivor would look like. So just being like very open minded to know how people might come in with different experiences and then being honest with them I think would definitely help a lot in terms of you know how to catch people while they’re, you know, in a place where they might need help.
21:19 Policies to Improve Trauma-Informed Care
Anne: So I was also wondering if you could tell us if there are any policy or changes that you think would improve trauma informed care in medical settings as well.
Abbey: Good question. I think in an ideal world, and if there were enough resources and enough time because I know y’all are also so overworked. Every medical professional if not to get 40-hour-trained but at least to get basic domestic violence or intimate partner violence training so that they’re able to identify domestic violence survivors or if someone discloses to them, like, knows what they need to do to be able to refer that survivor to the resources or services that they might need. And then I also think just increase partnerships between domestic violence organizations and hospitals, or like medical groups. I know that there are a lot of domestic violence agencies in the Chicagoland area who have partnerships with certain hospital or medical groups in the Chicagoland area where those hospitals provide
reduced cost or just like no cost care to survivors if they were to come into the hospital requiring care after experiencing domestic violence. I also know that there are really strong referral networks so if a survivor, if someone comes into the emergency room after having experienced really severe physical domestic violence, a nurse has the knowledge and knows who to call, and can know how to speak to the survivor and ask, “Hey, like, do you want me to call a hotline with you?”. And then, since they have that like referral network and those partnerships with these DV organizations, then also medical staff know who to call. And I think also, this is more like a policy level unless on like an individual medical professional level but ensuring federally like nationwide that all people have affordable health care. And so that people aren’t afraid to ask for care. I think that is one of the biggest barriers as well like “Oh, how am I going to pay for this if I were to go in to ask for testing, screening, medication, etc”. And a big part of our advocates work at KAN-WIN too, is trying to find as much as possible, state or government assistance for our survivors because a lot of our limited English speakers or might be low income or don’t have a lot of financial independence because of the abuse that they’ve been enduring so short answer to all this is just more, more just policies for all people and then also stronger partnerships and collaborations between the medical field and domestic violence field.
Anne: Yes, I totally agree with all of that like just like the stronger partnerships like I mentioned before working within the community I think it’s so powerful, because you know like, if y’all like KAN-WIN have a great network with people that you know are seeing survivors with clients, then you know, having medical groups partner with you guys really just capitalizes on that sense of trust and can really more effectively like help you all with your mission and like approach people who are survivors of violence in a way that’s familiar to them, safer for them. And then, in addition like you were saying with the policies, especially the financial aspect that you were mentioning, I think that’s huge, just removing that burden kind of opens up a whole new world, or it makes it so that people aren’t afraid to ask for help if they need it.
24:42 How to Connect with KAN-WIN
Anne: And then, just kind of as a last question, I was wondering if you could let listeners know where they can hear more about KAN-WIN’s work. What are ways for them to get involved and any exciting kind of new services or programs that you guys are doing.
Abbey: Yeah, so best way to stay updated on our work is to follow our Instagram. Our handle is @KANWINChicago, all one word, no spaces or underscores, and our website is KANWIN.org And you can subscribe to our newsletter there, our website also regularly updates like news and updates. So, great way to stay updated on the work we’re doing.
25:47 Wrap Up
Anne: Great, thank you so much for speaking with me today, sharing with us, you know more information about how to interact with survivors of violence, especially the tips on trauma informed care and culturally responsive methods. I think this was a great conversation, I learned a lot, I hope that the people listening learn a lot too. Yeah, thank you again so much for meeting with us and sharing today.
Abbey: Of course, thank you so much for having me and coordinating this, it was an honor.
Response to Proposed Limits and Elimination of Federal Student Loans
On April 28, 2025, Congress released a draft proposal to overhaul the federal student loan system, aiming to add limits to federal student loans, eliminate Grad PLUS loans, and drastically scale back current repayment plans and loan forgiveness options. For 75% of medical students who take out federal loans to pay for medical school, these new proposed rules will stifle the training of future physicians in a nation already facing a physician shortage among a growing and aging population. Congress is also discussing changes to reduce Pell Grants, which help fund undergraduate education for low-income students, including pre-medical students.
APAMSA’s membership is made up of over 4,500 medical and pre-medical students from across the country, and our national organization opposes these alarming changes that will irrevocably damage medical education financing for tens of thousands of medical students and for the many other health profession students.
We urge students to spend 5 minutes of their time to reach out to their Congressional representative to demand the protection of federal student loans. Please send this to your fellow classmates – more people contacting means higher importance to our representatives.
To find your Representative and Senators, please use the following website: https://www.congress.gov/contact-us
We have provided scripts that you can use in an email or in a short phone call to deliver your concerns about the proposed changes. Please feel free to adjust these scripts as you wish to better express your concerns. If you have voted for the Congressional representative or senator before, please mention that as a part of your statement.
Version 1:
Hi, my name is [NAME] and I’m a constituent from [CITY, ZIP].
Thank you so much for your continued support of our medical students and the future patients they’ll serve, especially in rural and underserved communities. I’m reaching out today not just as a student, but as someone who grew up in [brief personal background] and who relies on the Grad PLUS program to afford medical school. If this option were taken away, students like me would be forced to reconsider whether they can even afford to complete their training—despite our deep commitment to serving communities in need. I remain concerned about proposals to eliminate Grad PLUS or impose borrowing caps below the true cost of medical education. These changes would severely limit access for students from all backgrounds and risk worsening the physician shortage in the very communities that rely on us. I respectfully urge you to continue advocating for policies that protect access to medical education and ensure that future physicians can continue serving the communities that need us most. Thank you again for your leadership and for considering the impact this would have on students like me.
Version 2:
Hi, my name is [NAME] and I’m a constituent from [CITY, ZIP].
I’m calling to urge [REP/SEN NAME] to protect funding for the federal student loan program and oppose the elimination of Grad PLUS loans and other loan repayment options. As a [medical student/pre-medical student] at [your school], access to federal student loans are crucial to the training of America’s future physicians. In order to provide the best care to our patients across the nation, we must be supported in our education.
Thank you for your time and consideration.
IF LEAVING VOICEMAIL: Please leave your full street address to ensure your call is tallied.
For questions regarding this statement, please contact:
Rapid Response Director, Brian Leung at rapidresponse@apamsa.org
Editor Director, Christine Le at editor@apamsa.org
Director of Organized Medicine, Jennifer Deng at organizedmed@apamsa.org
Statement on Lapu Lapu Day Festival Tragedy
The Asian Pacific American Medical Student Association (APAMSA) extends its deepest condolences to the Filipino Canadian community in the wake of the devastating tragedy at Vancouver’s Lapu Lapu Day festival. On April 26, 2025, a vehicle was driven into a crowd celebrating Filipino heritage, resulting in the loss of 11 lives and injuring over 20 individuals.
This senseless act has left an indelible mark on a community that was gathered together in joy and cultural pride. As future healthcare professionals committed to serving Asian American, Native Hawaiian, and Pacific Islander communities, we stand in solidarity with those affected. We honor the resilience of the Filipino community and the dedication of the first responders and healthcare workers who provided immediate care and continue to support the victims and their families.
APAMSA reaffirms its commitment to fostering safe and inclusive environments for all communities. We pledge to advocate for mental health awareness, community support systems, and preventive measures to ensure such tragedies do not recur (Resolution 30.001). In this time of mourning, we offer our support and stand united with the Filipino Canadian community.
For more information on how to help, please look to Filipino BC (@filipino_bc) and at the official City of Vancouver website for more updates and ways to support the community in the future.
If you or someone you know needs support, please reach out:
988 Suicide & Crisis Lifeline: Call or text 988 (24/7, nationwide)
Asian Mental Health Collective – Resource Directory: asianmhc.org/resources
Crisis Text Line: Text HELLO to 741741
For questions about this statement, please reach out to the National President, James Chua at president@apamsa.org, the Southeast Asian Director, Fern Vichaikul at sadirector@apamsa.org, or the Rapid Response Director, Brian Leung at rapidresponse@apamsa.org.
Personal Statement and ERAS Workshop

In this episode, Dr. Grace Kajita, Dr. Indu Partha, and Dr. Sreekala Raghavan share their expertise on crafting a compelling personal statement and navigating the ERAS application process. They discuss key strategies for standing out in a competitive residency cycle, common mistakes to avoid, and what program directors are really looking for. Tune in to hear their practical tips, real-world insights, and thoughtful advice on helping your story shine – whether you’re applying yourself or mentoring the next generation of physicians.
Listen here:
This episode was produced by Annie Nguyen and Ashley Tam, hosted by Tanvi Chitre and Mason Zhu, and graphic by Callista Wu and Claire Sun.
Time Stamps:
0:00 Introduction to White Coats & Rice: An APAMSA Podcast
1:16 Introduction to Drs. Grace Kajita, Indu Partha, and Sreekala Raghavan
3:15 Mastering Letters of Recommendation with Dr. Indu Partha
10:50 Telling Your Story Through ERAS Experiences with Dr. Sreekala Raghavan
23:26 Crafting a Personal Statement with Dr. Kajita
30:46 How Should I Approach the “Hometown” Section?
33:09 How to Use Program and Geographic Signalling
35:53 Virtual Open House Etiquette and Post-Event Follow-up
39:58 Potential Red Flags in Applications
44:18 Letters of Recommendation – What to Consider and How Many to Get
48:54 How to Find Virtual Open Houses for Internal Medicine Residency Programs
51:04 Should I Mention Subspecialty Interests in My Personal Statement?
54:33 Event Outro
55:14 Closing
Full Transcript
0:00 Introduction to White Coats & Rice: An APAMSA Podcast
Annie: Welcome everyone to the 10th episode of the Asian Pacific American Medical Student Association Podcast. From roundtable discussions of current health topics, to recaps of our panels with distinguished leaders in the healthcare field, to even meeting current student leaders within the organization – this is White Coats and Rice. My name is Annie Nguyen, a postbac at Stanford University, and a member of the Leadership Committee here at APAMSA. I’ll be your host for today!
In this special workshop episode, we’re joined by three incredible physicians—Dr. Grace Kajita, Dr. Indu Partha, and Dr. Sreekala Raghavan—to dive deep into the art and strategy behind crafting a standout personal statement and mastering the ERAS application.
Whether you’re prepping for residency applications yourself, or mentoring students who are, this episode is packed with invaluable advice, real-world insights, and actionable tips to help your story shine. From dos and don’ts to what program directors are really looking for, our panel covers it all with warmth, honesty, and unmatched expertise.
Today’s episode was moderated by Tanvi Chitre, a medical student at the California Health Sciences University and Mason Zhu, a medical student at the Georgetown University School of Medicine. Both are members of the 2024 Leadership Committee.
1:16 Introduction to Drs. Grace Kajita, Indu Partha, and Sreekala Raghavan
Tanvi: Welcome to our Personal Statement workshop. We’re so glad to have you here. And, um, we’re really glad to have our three amazing speakers who will be answering all your questions and sharing all their knowledge about the residency process. And this workshop is brought to you by the National APAMSA Leadership Committee. So hope you enjoy! So our three speakers are Dr. Grace Kajita, Dr. Skreekala Raghavan, and Dr. Indu Partha. And they’ll be talking about different aspects of the residency application and also doing a Q&A with everyone at the end. Doctor Raghavan, if you wanted to introduce yourself.
Dr. Raghavan: Yeah. Thanks so much. Um. I’m Skreekala Raghavan, I am an associate program director for internal medicine residency at Mount Sinai Morningside in West, which is in New York. I’m excited to be here and joining you guys today.
Tanvi: Thank you for having– for coming. And Dr. Partha.
Dr. Partha: Hi, everybody. I’m Indu Partha. I am also an associate program director for our internal medicine residency program here in Tucson at the University of Arizona College of Medicine. I’m super excited to be here, and I’m thankful to the organizers for putting on this event.
Tanvi: Great. We’re so glad to have you. And finally, Dr. Kajita.
Dr. Kajita: Sorry I had a little trouble unmuting there. Hi, everyone. It’s nice to meet you all. I’m Grace Kajita. I am the program director for the internal medicine residency program at Montefiore Medical Center, specifically the Wakefield Track. And for those of you who don’t know where we are, we are actually in the Bronx, New York. Thanks so much.
Tanvi: Perfect. Thank you all. So this, um, is the little snapshot of what we’ll talk about in this presentation. We’ll cover letter of recommendations, experiences, and the personal statement. And then lastly is the Q&A.
3:15 Mastering Letters of Recommendation with Dr. Indu Partha
Tanvi: So we’ll start off with Dr. Partha for the letters and rec.
Dr. Partha: All right. Thank you so much Tanvi and Mason and Reanna for the invitation. And I’m super excited to talk to you guys about letters of recommendation, I think. Um, a couple of things I’d like to go over is when to ask for these recommendations. Um, who to ask for the recommendations and what to ask them, um, to actually do for you. So I think one of the hardest things for any student is just the anxiety that is related to asking somebody for a letter of recommendation, and I wish there was a way I could tell you that, you know, this is an easy thing. I think depending on different people’s personalities, um, and their interactions with their faculty and attendings, um, it can be easier for some, harder for others. But I want to reassure all of you guys that from a faculty standpoint, we all recognize when it is, um, time for applications to be turned in, we understand and know that our students are going to need letters of recommendation, um, from us. I think those of us in internal medicine especially, is one of the core clerkships are quite, um, used to having students approach us. So I don’t think you need to worry that this is a shocker to an attending that you’re going to be asking, and so at least feel a little bit reassured in that, you know, why is it important to ask the right people and make an effort to get a good letter of recommendation is, truthfully, you really want it to be a personal and non generic letter. Um, yes, letter writers are doing a lot of letter writing during application season. Um, but there are ways and I’ll go over some of those tips that I can offer you to help you create a more– personalized letter for yourself. Because in this day and age of AI, I think more and more letter writers are incorporating AI to help them write these letters. So what is it that we, as the folks asking for letters, can do to help improve our success? One of the biggest things, though, I would advise you all, is be mindful of who you’re asking for a letter. Um, make sure that this is someone who has seen you, you know, perform your best. You want to set yourself up for success, and it’s totally appropriate when you’re first meeting an attending on a on a clerkship that you know you need a letter from is just a straight up at the end of your first day to say, you know, “doctor so-and-so, I would really like to get a letter of recommendation from you at the end of this week because I’m applying for residency and XYZ– what would you recommend or what would you like to see for you to feel comfortable writing me a very strong letter of recommendation?” Um, and that’s going to be a clear ask. You kind of want to make it, um, apparent to your writer that you’re going to ask for a letter. You want them to know what you know. If you’re applying into internal medicine or surgery or what type of residency program you’re applying to. And once you take that next step and reach out with a letter in follow up. You can most certainly be a little prescriptive on what your hopes are of what they would like, what you would like them to focus on. For instance, you might have one attending who really saw you at your best in your interactions with patients, in your clinical care. You might have another attending who you’ve done research with, who can really speak to your scientific prowess, and another one, perhaps, who you did some type of procedural elective with, who can speak to your technical skills. So it’s perfectly okay and appropriate to ask each letter writer to focus on perhaps a different aspect of your skill set to highlight for your future programs to review. So, you know, you’ve settled with doctor So-and-so that they’re going to be willing to write you a letter, so when you write them a formal request via email, it’s helpful to be ready with all the information that they would need from you. And this is that kind of helpful information. You want to send your CV. You want to send a personal statement so they understand all that you have done already, what your personal statement and your ideology is. I know you guys will be getting some good tips here on what to include in that personal statement. Um, what I tell my students to include or residents when they’re applying for fellowship is, um, do you have evaluations that are from other rotations, from other classes that speak to how well you’ve done? All of that information can help show your letter writer what a well-rounded student you are. And I would include all of those. I would be very clear on what your deadline is. I would I need this letter to be submitted to ERAS by whatever my tip would be to put that deadline a week or so before your actual deadline, so you’re not scrambling towards the end. Um, perhaps ask them if it would be okay for you to send them periodic reminders. A lot of letter writers truly want to do right by their students, but just are so busy that they would actually appreciate getting some, um, reminders. And lastly, I would encourage you to provide some answers to some questions that I’ll review over to help you, um, personalize your letter. If I could get the next slide. I didn’t want to over text this, so I’m going to read these off, and you guys, if you feel like this could be of help and, you know, note them down. Um, I want to credit Dr. Kimberly Manning for, um, this idea. I’ve used it a lot for my letters that I’ve written, and it’s really helped me, uh, create some personalized letters. What I would do is when you write to your letter writers, you can tell them, you know, my mentor suggested I provide you some of these answers to help you in your letter writing to make it easier for you. Um, and the questions I have for my students answer is: “what are your strongest attributes and what are you most proud about yourself? Um, What have you done that could set you apart from other applicants? How would your peers or teammates describe you? What would you want to make sure the programs know about you and your candidacy? And then this is an optional one – what hardships, um, if you’re open to sharing, have you experienced that might cause you to be misunderstood? Again, totally optional and different students have different experiences. And lastly, three words you would like to see in your letter in support of your candidacy.” Um, if you provide answers to this and send it to different letter writers, just a reminder, please change your answers for each letter writer so they’re not all writing the same letter for you. But I have found utilizing my students answers to be very helpful for me personalizing their letters. Um, my last thing I would say is this isn’t the time to be humble. Utilize impactful words and language and be clear about what you’re proud of and what you have done. Um, this isn’t the time to, uh, sort of downplay your skill set, because this is your chance for your letter writers to advocate on your behalf. Thank you very much.
Tanvi: Thank you so much, Doctor Partha, for all of that.
10:50 Telling Your Story Through ERAS Experiences with Dr. Sreekala Raghavan
Tanvi: Next we have experiences from Doctor Raghavan.
Dr. Raghavan: Thanks so much again. Thank you for having me here. This is you know, the section about experiences in ERAS has changed over the last number of years. And so I think the way that programs have been using this section has evolved over time. And so I anticipate a lot more questions will come up than just what I’ve answered here. But what I’m really going to talk about. Um, before the Q&A at the end is what should you really include in your experiences? What should you consider leaving out? Um, and in that ERAS section, what are the most meaningful experiences mean, and how do you select which ones they’re going to be? And then what– you know, what are really– what are what’s really being sought, uh, in that impactful experiences session, which is different than most meaningful. So, you know, you can probably guess that they’re looking for different experiences that you’ve had in, uh, in the ERAS- in this ERAS section, and that includes a bunch of pre-selected categories that you can select through, uh, the ERAS application itself. I’ve kind of highlighted some of them and combined some of them a little bit here, but a lot of them are the activities that you’ve taken on potentially as clubs or extracurriculars while you’ve been to medical school. Um, a lot of folks talk about the work that they’ve done. As it’s become increasingly popular to take time between medical school and residency, and some folks may have worked as a scribe or done their certification to be an EMT and worked as, uh, as an EMT, even customer service roles and and roles that are not directly related to medicine and the medical field are, you know, can highlight a lot of really amazing things about you, characteristics that you have or skills that you’ve built while doing that job. Um, and so these are kind of the, the larger areas that you want to talk about. Some particular things for– I’m not sure exactly sure who is in the audience– so just to point out, uh, for folks who either took a lot of time off between, um, college and med school or you’ve had a little bit of a, um, like you don’t have a standard 4 year timeline for medical school, you want to be sure to use your experiences to really build in the timeline. So this very often applies to folks who are going to medical school outside the US and uh, and coming to do residency in the US, where they may have graduated medical school some time ago also, and have some years, um, in between. So if they’ve done clinical experiences in the US as observerships or, um, any externships, hh, they should definitely list– you should definitely list all those experiences because as a, you know, on the program side, what I really want to know is what’s been happening during all of this time in between and what how are you learning and growing and changing and then kind of beyond that, um, what you’re really using this section to do is to highlight who you are. What are you passionate about? Um, you know why medicine, right? So you’re going to talk about why your particular field, why you went into medicine in general, um, in your personal statement. But this is where you kind of highlight all the activities that led up to that, the kind of evidence behind all the, uh, the larger statements that you make in your, in your personal statement. And when I’m reviewing experiences, I really want to know what you’re passionate about. So then, you know, you’ve done quite a lot of things, I’m sure, over, over the last number of years. So how do you decide which are the ones that you’re going to include? You can only include ten, and you can only mark three of those ten as your most meaningful experiences. So I would you know, when you’re really thinking about which those ten are, you want to highlight things that highlight that passion, right. And you want to choose things where you’ve really shown some sort of a commitment. You certainly want some if you have had leadership positions, for example, these folks, lovely folks who are running this workshop today as part of APAMSA leadership. So highlighting that, um, type of, uh, work that you’re doing through– or service that you’re doing rather– um, through your activities is really, uh, a way to, to separate yourself, right, to, to show how unique you are, uh, in your application. Hobbies? Also, I don’t have it as a separate section here, but hobbies do fall into this experiences section. Sometimes, uh, hobbies or work or significant activities, especially for medicine before your life in medicine, um, matter. So if you were, um, like a concert violinist for a bunch of years before you really got to this point, it highlights a lot about who you are– dedication, um, different skills that you build, um, potentially around problem solving, around dependability. Um, and so all of those characteristics that you want to show, if you want to show that those are the things that you’re strong in. And these activities can help you to highlight that. Um, this is not a CV. Uh, and so just to remember that, uh, you really want to pick these, these things that highlight exactly what– what helps you stand out from the, uh, larger pool of applicants. So then how do you move into selecting your most meaningful three? Answering those questions that, um, that I mentioned a little bit earlier, like: “Who are you? What are you most passionate about? And which were the activities that helped you grow the most?” That’s also really, um, impactful when I read it. Not impactful in the ‘Most Impactful’ on the experience that I’ll talk about a little bit later. But, um, when I’m reading an application and I see that, uh, somebody has a clear theme in the things that they’ve found to be meaningful, that they’ve really grown a lot, um, participating in particular activities. It helps me feel out whether this is somebody who’s going to thrive in my residency program environment or, um, not maybe enjoy taking care of the particular population that we take care of, um, or not, or want to focus on some of the additional opportunities that exist within my program. So I’m really looking, not just for somebody who qualifies kind of on paper as like a top student. I’m looking for somebody who really wants to train with me and wants to be in the environment that my residents are in. They’re going to have a great time and learn a ton of medicine and be great at the end of it. So those are, you know, the showing your growth through your meaningful experiences, I think is a really great way to highlight who you are and how you fit in your particular, um, learning environment.
Dr. Raghavan: So what do you not want to include? Um, this is not a place to list and to have an exhaustive list of every single thing you’ve ever done. Um, some of the questions that often come up are, should I include things I’ve done in college? Yeah. I mean, if you did something for four years in college, you showed a real commitment to it. You had a leadership position in it, or you did something for a while between, um, between college and medical school. These are all things that you can include. So just the actual timing of it. Like the number of I mean, the year in which you started doing something is not or determines if it’s a really old activity. But if you volunteered for someone or something for three months in your freshman year of college, that does not go in your experiences section because it doesn’t really speak to who you are now as you apply for residency. Looking into like something that you participated in at one time, if that one thing was, you know, something that was really, really meaningful to you because it challenged you in a particular way and you grew, you could make a case for including something like that. But typically you want to– you want to show that you were really passionate about something and that it made an impact on you. This is not a place to list your abstracts and your manuscripts. There’s a separate research session for that, but that question does come up quite a lot when you list your research experiences, what you’re listing is what you learned through participating in research, not the abstract that came out of it, not the manuscript that came out of it, but what were you working on? What was your role? And so that was one of the other things not to include– if you really don’t remember what you did in a particular activity, it probably didn’t mean so much to you. So don’t put that down there. You will, you know, anything on your ERAS application is fair game in your interview. And so if you put down something that you’re not prepared to talk about, um, interviewers can be surprised and feel like, oh, even though you highlighted this was one of your 10 activities and you can’t really talk about it, they’ll question the veracity of the statement also. And so you don’t want to get caught out on that. And then again, not just that you don’t remember your role, but that you can’t describe the activity or the experience in detail because when questions about experiences come up, it’s often, you know, “what did you learn from that experience? How did you grow? What challenges did you face?” And you need to be able to describe all of those things to be able to to really show your passion and show how you stand above the crowd. And then finally, you don’t want to overlap everything with your personal statement or with the content that you go over, uh, typically with your student advisor that goes in your medical student performance evaluation or your MSPE. If they’re all exactly perfectly aligned, you just have a lot of repetition in your, uh, in your application. So you want to, you know, use this as an opportunity, this section as an opportunity to highlight other things about your commitments.
Dr. Raghavan: And so then the final question that really comes up about, um, about this section is that there is a separate question about impactful experiences. So meaningful is the meaningful experiences that you highlight, which are three of your ten experiences are the things that you know you really want to show that you are passionate about. Impactful experiences, not everybody will necessarily have to answer to know, what the question is really asking is whether you had any real obstacles during, you know, during medical school or potentially at a time before medical school kind of leading into your career as you start. Um, and so if there was something that really impacted your journey and maybe made, uh, made that distance traveled greater if there. You know, very commonly we see, uh, personal illness stories in this, uh, in this section, you may see, um, other kind of, uh, socioeconomic difficulties of getting into, um, a particular track or into medicine, um, listed in, uh, in the Impactful experiences section. But, uh, by and large, most students are not actually filling out this, um, this section because you don’t– this is not a standard section that we expect to see something in. This is a way to explain something that may have affected your– your path as you were on, you know, on your way to where we meet you, um, and that you had to overcome. And so it helps, uh, it helps us to see who you are a little bit differently, and how you arrived at the place that you are at and understand, you know, what hardships you really had to, had to kind of go through. Um, and then just to remember that you don’t have to explicitly state that your impactful experience, uh, had, you know, had something to do with your meaningful experiences. But if you overcame a particular challenge and then you volunteered for a foundation that helps folks, um, overcome such a challenge, or you have a leadership position and something like that, it’s clear to kind of see that, um, as a full circle without having to necessarily, uh, list it out in your application.
Tanvi: Thank you so much for that comprehensive look on how to figure out what, um, experiences to include.
23:26 Crafting a Personal Statement with Dr. Kajita
Tanvi: Um, finally, we have Doctor Kajita with the personal statement.
Dr. Kajita: So I am super lucky because I’m following two really excellent speakers who really have said so much about what makes the foundation of a personal state. And you’re going to see a lot of themes repeated in what I’m about to say. The personal statement for some reason has, at least in my experience, turned into this somewhat painful exercise that everyone leaves until the very end just before they submit their application. Because it feels big. And I want to let you know that you don’t need to do that. You can start it right away. You can work on it in bits. It doesn’t have to be painful, you just want to get started. The second thing I want to say about it, that I’ve learned in my experience, from talking to people who are applying largely for fellowship, that I think people feel that there’s some sort of way that you can read the mind of the person who’s going to be reading your personal statement and sort of craft something for that person. Note that this is a personal statement. This is about you. And honestly, all of us who are reading a personal statement really just want to know about you and know about what you care about and know why you’re here. So don’t feel that there is an absolute formula or that you’re trying to quote “game the system”. Write your personal statement about yourself using many of the tips that have already been discussed. And so when I say make it personal, do all the things that Dr. Raghavan just said about what you want to include and keep it simple. You really don’t need to include everything about your life, as long as it’s all really about you and in your voice. One of the things that we tend to do is we tend to be a little bit modest. Please give yourself credit for what you’ve done. You’ve made it this far. You are all really impressive people. Be proud of that. Share that. We want to, we want to know about that. And when giving yourself credit. This is not about itemizing all of your accomplishments. This is about really saying something about yourself, particularly maybe what you’ve been proud of, what has brought you to medicine. Don’t repeat your your CV. And because you want this to be in your own voice, do not. Please do not use ChatGPT or AI. This is a whole new frontier. They’re probably going to be better rules about how to use it in the future. It’s okay if it doesn’t sound like classic literature. This is you again. Be honest and don’t stretch things to make it sound more impressive, because that’s how– so the Olympics are on. You can say, I played soccer in college, but you don’t have to turn it into. I was on the Olympic stage, right, because someone’s going to ask you about it, right? Only include stuff that you can really talk about. It’s okay. On the same note, to not have too much stuff in there. This is about quality stuff. Okay. It doesn’t have to be two pages. In fact, you want to keep it one page. You want to keep it tight. You want someone to read it. For typos and proofreading and for how it’s phrased right? If your reader is a friend, maybe it can be honest with you and faculty and say, this is kind of boring, you’re kind of trying too hard. That’s okay. That’s why you’re going to give yourself time at the beginning, because it’s like crafting any good, any good essay. It’s going to take multiple rewrites, but don’t be intimidated by it. You can all do it. You all done statements like this before.
Dr. Kajita: Now some people have some questions about how to format your personal statement. What do I start with? Is there any one way to do it? There really isn’t. I usually tell people. Um, you can start with an anecdote if you like, but we are always– thank you for your advancing the slide. Um, and that’s often what people do, and to a point where it’s almost become a formula, but it can be a positive. It’s a good way to start. Maybe that’s not where you end up, but the classic to the point that as readers, we sometimes kind of all, um, laugh or in a kind way, mind you? Oh, this is familiar. We know where this is going. Phil and the family member had a heart attack. Ended up in the emergency room. You did CPR on the field? They- they survived. And this is why you want to become a doctor? Okay, that’s great, but it’s not necessary. Some of you have never had this kind of crisis. You may have other reasons. Do you not feel that you have to fit things into a formula. Similarly, I get asked this a lot and I see it done well sometimes and not so well. Think about whether or not you want to start your essay with a quote from Doctor William Osler, because it’s a medical quote– don’t do it to impress us. Do your quote if it’s something that really means a lot to you, okay. And the quote doesn’t have to be a famous person, but we’re also used to seeing the quote that my grandfather said, fill in the blank. That you should become a doctor. Okay. You don’t need to do that either. Okay. It means a lot to you, and you can tell a story. Which includes things about why you are the right person for this particular residency. Go ahead. Okay. The reason why I say maybe or maybe not on this slide is because I put it out there and then have someone look at it and see if it seems genuine. Okay? Because this again, it’s about you. Please do not recycle your med school applications. Okay? I see people do this, and you’re already so much more impressive by the fact that you’ve gotten into med school and you’ve done all of these things. You’re not the same person. Not just in accomplishments, but in your insights and your personality. You’ve grown. Please don’t recycle the old application. Finally, some people have asked, well, I really want to stand out. I want to do something different. People try to do things like write essays in iambic pentameter. One wrote an essay about, um, going to Shake Shack. Okay, this is a real essay. Okay. It was a remarkably successful essay, but that doesn’t mean that it’s the best essay for you. It might be entertaining, but it might not be what the program director is looking for you. Remember, this is a representation of you, and we’re not looking for fireworks– were looking for you. So please, if you are an amazing writer, you have a talent for it, go ahead. You know, this is one of those things that you want to include in your experiences or really makes you stand out. Be my guest. But it’s not necessary. Use good judgment about these things. And always, always. A lot of people want to help you succeed, and we are a friendly audience, so please, please don’t be afraid to share your work before you submit it. And that’s all I have to say.
Tanvi: Thank you so much. Um, the personal statement is always a huge obstacle to overcome in these applications, so your advice is very helpful.
30:46 How Should I Approach the “Hometown” Section?
Tanvi: Um, next we have some FAQs. Um, first, what to write for hometown. Um, if anyone wants to address that.
Dr. Partha: I might just speak up only because, um, I think between me, Doctor Kajita and Doctor Raghavan, I am from a program in a relatively smaller town and a less populous state. So the only advice here I would have is, you know, we don’t need ten different hometowns of every place you have ever lived. However, where this can be somewhat useful for programs like mine and Tucson where yes, we do kind of look through and see what an Arizona connection might be because, you know, we want applicants who are really serious about coming here is if you did not go to undergrad or medical school in a particular state or location, that’s a bit smaller, but you do have some connection, like maybe you did live here, you know, between birth and sixth grade, I, I think that can be helpful to signal to a program in a smaller location that, hey, I actually do have some connection to Arizona. So me living in Iowa right now, applying to Tucson isn’t as crazy as it might look. Even though I went to undergrad in Michigan and medical school in Chicago, and I grew up in Iowa, that’s where my permanent address is. So sometimes the hometown, if it’s a legitimate connection to a place, might be a great way to sort of slide in a little bit of an indication to a program in a less popular location or city or state that you do, in fact, have a, uh, a connection, a personal connection to that place.
Dr. Kajita: So if I could add a comment to that. People have lots of options. You can fill in more than one hometown. But going back to the whole issue of is it meaningful? Remember, if someone’s going to ask you about your hometown potentially. So make sure it really is a substantial connection to that town, and not just the two months you spent there on vacation with your family because you want to impress someone.
33:09 How to Use Program and Geographic Signalling
Tanvi: Um, next, is it useful to apply to many more programs than number of signals you have as an applicant? Um, and geographic versus program signaling. Thoughts?
Dr. Raghavan: I think this. Um, so all three of us happen to be from internal medicine. Um, and so the I think the answer to this question really varies based on the specialty that you’re applying into, um, in internal medicine, it’s typical to apply to many more programs than the number of signals that you have. Um, most folks are applying pretty broadly, you know, whether that’s in a particular geographic region or not, or if they’re just applying widely around the country. That’s um, that’s very normal in internal medicine, in other, um, in some really competitive fields. Uh, a lot of programs actually, uh, do look really mainly at the folks who have signaled them. So I know in dermatology this is a significant, um, way that folks try to limit the number of applications that they’re reviewing. Um, and so a lot of dermatology programs, especially in very populous cities, um, do use the signals as a way to essentially say, these are the folks that I’m going to really review first. Um, they may continue to review after, um, but if they fill their number of interview slots with folks that have signaled them, those are going to be folks that are really getting that preference in a, in a very competitive field. Um, and then geographic versus program signaling again in very, very competitive, uh, fields. I think program signaling really carries the strength over geographic signaling. Whereas, um, in fields like pediatrics, family medicine, internal medicine, um, there are or kind of larger number of programs, um, geographic signaling carries a significant amount of weight, because if there are a large number of programs in a particular field, in a particular, uh, area, you may not be able to signal all of the programs in that area, even if you’re very interested in living in that particular area. And so programs that have, uh, or specialties that have a lot of programs in a particular, um, area may use geographic signaling even maybe preferentially over program signaling. Um, and then finally, the competitiveness, I guess, of the actual program itself also determines, to some degree, the answers.
35:53 Virtual Open House Etiquette and Post-Event Follow-up
Tanvi: Okay. Thank you for that. And finally, um, what is good etiquette for attending virtual open houses? Maybe doctor Kajita, if you wanted to take that one.
Dr. Kajita: Sure. And I’m sure the people will have some opinions on this. I think the main thing is that you are present, that you are courteous to not just the faculty, but your colleagues. I found that at some open houses, it it turns into a little bit of a competition to impress. Just if you have a question, ask. And certainly, um, collaborate with the– your co-participants because you’re going to be seeing a lot of each other on the interview trail. It’s important that you can start some of these relationships now. Um, do all of the appropriate things that you do on a zoom call and all of those things in terms of muting and not muting, not having a lot of noise in the background, those kinds of things that you would do in any type of meeting. I’m not sure what specifically this question was addressing Reanna. I think you were the one who brought it up. Is there anything in particular that we can answer for you?
Reanna: I was curious more along the lines of like, reaching out to programs after you attended an open house, or what’s the etiquette there? Because I know contacting programs, you don’t want to contact them too much, but if something’s meaningful. Like how do you approach that?
Dr. Kajita: Okay, that’s a great question. Um, my answer to that is I, I don’t mind at all, and I appreciate a short thank you. Um, however, I would prefer that once you thank me. Thank you, thank you. That, you know, you don’t need to continually send more thank yous. I’m interested in this. I like this so much about your program. A simple thank you is more than enough for me. And I’m curious as to what the other faculty think.
Dr. Partha: Yeah, I would agree. And I would say, etiquette wise. Um, the thing to remember is, granted, there might be a lot of people on line, but, um. You can be remembered both for being positive and for being negative. You know, some of the residents who are online definitely give feedback. Oh, this one student was really, you know, whatever XYZ either positive or negative. So if you’re really serious about a program and are showing up to the open house, I would say bring your A game, know about the program, be a little bit ready with some really good specific questions to indicate, hey, I’ve really looked at your website and know about your program. Um, and those are ways to kind of set yourself up a little bit so that, um, if like a chief resident is online, there’s no faculty, that chief might say, oh, there was, you know, a student named Reanna. She really seemed very interested and super excited and polite and, um, you know, we’d love to have her versus, oh, gosh, there was this one student who all they were concerned about is how many vacation days they’re going to get. And what’s the days off? Um, and so just realizing that what you’re saying can often really help or sometimes, unfortunately, um, be negative for you.
Dr. Raghavan: I also want to highlight that it’s a little bit of a first-date situation and you are also assessing the program. Right? This is usually your slightly more extended way to hang out with some of the house staff or people currently in the program and get a sense of if these are people you want to spend a lot of hours in somewhat stressful situations with. And you want to– certainly you don’t want your questions to focus on the schedule and vacations, that’s usually included on the website or materials on your recruitment day, but really get to know what connects people in the program and showing that level of interest, so showing that you know a lot about the program for sure but showing a level of extra interest of what would it really be like to be in this program also can get noticed as a passion for that program.
39:58 Potential Red Flags in Applications
Tanvi: Okay, perfect, so last we have about 15 minutes left and we will do the Q&A session now. I think Mason and Reanna have been combining all the questions together so if you want to tell us the first couple questions.
Mason: Sure, I will bring those questions up. Thank you all of submitting your questions, we may not get to all of them but we will try to prioritize the ones that apply to most of the people. We got a question, I think it goes along the lines of what not to do that Dr. Raghavan mentioned about some of the open house etiquette, but for application reviewers, what are some of the common red flags that you will see on someone’s personal statement or their ERAS application overall?
Dr. Raghavan: I’m just going to say that if there is something that makes you stand out in a particular way, like you had to repeat something or you know there’s going to be a statement about something that is not the most positive in your MSPE which typically, medical schools now allow you to see even if you can’t edit– that should be explained somewhere. A red flag for me is not that actual thing, the repetition of a clerkship or something like that, the red flag is not knowing what happened and potentially– as a reviewer, I think, maybe the student didn’t realize this was significant and didn’t use it as a learning opportunity. But I want to see that there was reflection about it, that particular experience.
Mason: All right. Thank you. Dr. Kajita or Doctor Partha, anything to add?
Dr. Partha: I would definitely, um, emphasize what Dr. Raghavan mentioned. Yeah, you definitely want to see an explanation. And I don’t know that this would be a red flag, but perhaps something. Um, I think both to what? Uh, Dr. Raghavan and Kajita reviewed over what is meaningful experiences. If you know, someone just has a list of volunteer activities and they’re each just one day for two hours, and that’s what fills their application. Um, again, like I said, not a red flag, but perhaps, you know, this person might be stretching for experiences and working on quantity over quality, so it might just dilute the competitiveness of an application.
Dr. Kajita: I would agree with both those. And the only other thing which isn’t obvious is having a lot of mistakes right? On your– on your application. If you, you know, it’s a it’s an important thing to you. And if it feels like maybe you’re not paying attention or you’re not as careful as we would hope you would be if there were a lot of typos, grammatical errors, spelling errors. You spelled your own name incorrectly. I’ve seen that before. I would worry a little bit about that. So just. That’s an easy one. Just be careful.
Dr. Raghavan: The one random thing and I feel kind of silly saying this, but, um, see what your picture is saying about you? Like, is it a just a nice– nobody is looking for an expensive fancy picture, but, you know, do you have a nice expression on your face? Is your hair combed and are you looking put together? Um, for the most part we see great pictures. But every so often we do see pictures that kind of grab our attention. And that might not be really the way you want to grab a reviewer’s attention is by a picture that’s kind of, um, standing out for being a little too dramatic, or somebody just threw something on and and took a picture.
Mason: Great, great. Thank you. It sounds like, you know, be forthcoming, be honest with your application. And also double, triple check your your work.
44:18 Letters of Recommendation – What to Consider and How Many to Get
Mason: And we received another question, a couple questions regarding the letters of recommendation. Uh, one of the questions was just asking, what type of letter writer– what type of letter writers are recommended? Uh, if you have a research mentor versus clinical versus your clerkship director, and kind of what’s the recommended number of letters to get.
Dr. Partha: I mean, most oftentimes you’ll need three letters of recommendation. One of them might be your, you know, chair letter from your department, different schools. What have different people? Um, writing that letter in our, um, institution, it’s our IM clerkship director, and it’s co-signed by the the chair. Um, I would say most certainly you want somebody who’s going to be in, in your field that you are applying to. So if you are applying to surgery, you need a surgeon. If you’re applying to medicine, you need someone in medicine. Um, you definitely want to look for people who are going to be able to write a good quality letter, not someone that was, oh, they’re super well known in their field, but I worked with them for two days. Um, so for the sake of that, you don’t want somebody to give you, like, a one paragraph meaningless letter just because they’re a star in the field. So you really want to look for, um, quality letters and then from the specialty that you are applying to. And if you don’t have all the letters from that specialty, usually it’s going to be helpful to have, you know, folks who’ve had more of your core clerkship experiences who have spent a little bit more time with you. Um, but if you’re really passionate about research and that’s what your career is, um, going ahead towards, obviously I would definitely have your research mentor letter speaking to your skill set there.
46:13 Letters of Recommendation for Sub-I Rotations and Visiting Students
Mason: Great. Thanks. And, you know, just to piggyback off that question, someone else asked. Kind of relating to quality of letters for fourth year med students who are doing sub-Is and they’re rotating at your institution. If they don’t feel like they’re getting a lot of time with the PDs. Um, should they still try to ask the PD, or should they try to focus their attention and ask the attending that they spent more time with?
Dr. Kajita: I tend to be a fan of the person who knows you better. I mean, a PD letter– PD is also just so you know, they’re cautious, right? Because you know, they know sometimes that their letters carry some weight. And so unfortunately sometimes those letters hopefully the PD would be frank about saying that, you know, I think someone else might write you a better letter, but the person who knows you and has seen what you can do in your sub-I in an actual clinical setting, that’s great. I think for myself, if it’s a strong, um, faculty letter from your sub-internship.
Dr. Raghavan: I think that’s great. I would say the other part of that, and I agree with Dr. Kajita completely, is that in certain specialties that are smaller, a lot of folks will really a lot of the faculty will know each other from around the country because they network at conferences. And, you know, they’ve spent a bunch of time in that area of expertise. And so if they see a letter from someone that they know, even peripherally, they may reach out to that person and, and ask like, oh, what was it really like to work with this, this candidate that I’m really interested in? Um, and if the response is like, well, I got asked for this letter, I didn’t really know the person that well, um, that’s not so great. And it’s much better to have a letter from somebody who’s going to really, you know, stand in your corner and talk about why you’re the right candidate.
Dr. Partha: I might just add two for the student to double check what the culture is in that program. Because I know for us, like our PD does not write letters for visiting sub I’s. I mean, she will write them if she’s there attending, but if they’re rotating, you know, with me she’s not going to write a letter. So, um, versus students thinking that’s the culture and what they need to do, they should kind of check ahead of time what’s traditionally done or expected, but completely agree with Dr. Kajita and Dr. Raghavan, to ask the person you’ve worked with, not the person who has the higher job title.
48:54 How to Find Virtual Open Houses for Internal Medicine Residency Programs
Mason: Great. Thank you. Um, you know, we have three of you amazing PDS and APDs and, um, you’re all in the internal medicine, uh, area. So we have a couple questions that are a little more tailored to the IM residency. Uh, we had a question asking what the best way to find the virtual open houses for IM programs.
Dr. Raghavan: So there might be kind of different definitions of this, because there are the kind of meet and greets when you’ve applied for a program. So that’s going to come directly from the program and be highlighted to you. Um, otherwise, you know, different programs that have virtual open houses for larger groups of folks in a particular area from a particular background or, um, particular set of interests. Um, those will usually come out through interest groups, advertising to interest groups, or advertising to student advisors, or sort of through your medical school. Um, I know at Mount Sinai where I am, the way that, um, the programs really have a kind of pre, uh, before we’re– we’re able to see, um, IRAs before you guys finish, uh, submitting all your ERAS applications our virtual open houses are advertised to medical schools around the country to their to advertise to their students, um, so that they can join and see what our programs are all about. And we usually do kind of a combined, uh, virtual open house across specialties. And then we break out into breakout groups so that folks can meet those in their specialty.
Mason: I just did a quick search on Google and it seems like, you know, for internal medicine programs, they might be specific to the school. So, um, you might, you know, uh, you know, might have some luck finding the specific programs you’re interested in and then seeing if they have an open house. Um, I know some specialties, like anesthesiology they have and like a central hub that lists all the open houses. So I would think that might also be helpful as well.
51:04 Should I Mention Subspecialty Interests in My Personal Statement?
Mason: Um, another question for kind of internal medicine, but also subspecialty related in your ERAS or personal statement, should you include your interest about these subspecialties? For example, if you have a passion in, uh, cardiology or any of the other subspecialties.
Dr. Kajita: I’ll take the first crack at this one. Um, I think that that there are there are a group of people who know from day one what they want to be, and that’s great. And there are people who don’t know or think they know and change their minds. So when I read a personal– certain personal statements for residency and they come in wanting to do cardiology and then they change their mind, that’s okay. I think the more important thing is, is it a coherent personal statement that talks about them and why they want to do cardiology particularly? Right. 50% of them who come to me change their minds, but I don’t– the personal statement was still great. So, um, I think that some people worry that they will be pegged in a way that, oh, we don’t have those kinds of we can’t support that particular interest, or we have too many people who want to become this particular thing. So, uh, but you don’t know if this is a program you’re interested in, think about that as well. What is this program like? You also want to think about when you write your personal statement. In some ways, that may also help you think about which programs you’re most interested in and how you rank them, because sometimes that also helps to define what your future career goals are. So I would say there’s no sorry, I’m so ambivalent about everything, but there’s no hard and fast rule about that as long as it’s honest and it’s you.
Dr. Raghavan: I will note that sometimes programs use, um, specialty interest information to, um, like, if they have resident buddies that they pair you up with after the match. So when those kinds of shared interests to say, hey, you know, I’ve got a second year who’s also interested in cardiology, I’ll help you out. And so if you’re really, you know, very interested in that sort of match up, um, and it makes a difference to you and how you transition into residency, it could be helpful. But then there are definitely programs, probably not the majority of PDS that I know. Certainly when I was doing my own recruitment as a PD I didn’t use specialties to say like, I’m not going to, you know, rank this many people who want to go into cardiology or GI or something. Um, but there are definitely programs that do use that, um, that type of criteria where they want to have a mix of folks in their class. Somebody wants to go to pulmonology and someone going to allergy and not a class that’s like split into GI, cards, and heme onc.
Dr. Partha: Let’s keep in mind that when you interview on that personal statement, your program does not want to hear all about you being a future cardiologist. But first, why you’re going to be an amazing internal medicine resident for them. So just watch how you sell yourself, because that could be off-putting. If your whole interview is about your passion for cardiology when you’re not applying for a fellowship at that moment.
54:33 Event Outro
Mason: All right. Thank you very much. Um, it looks like we’re about to approach the 9:00 mark eastern time. Um, so that’ll be our last question. But, um, you know, first of all, we want to thank Dr. Kajita, Dr. Raghavan and Dr. Partha for coming and speaking about the IRAs and personal statement and really helping us neurotic third and fourth year med students and aspiring physicians kind of, um, get their bearings. Um, I believe, uh, our panelists have also agreed to share their emails or contact information. So, you know, if you have any lingering questions or interests, you can feel free to reach out to them as well.
55:14 Closing
Annie: And that’s our latest installment from the Leadership Committee. If you have a specific topic or specialty you’d love to hear more about, please let us know. You can reach us at professionaldev@apamsa.org. We hope you enjoyed today’s episode as much as we did, and don’t forget to tune in next time! Thanks everyone!
2025 National Conference Posters
Congratulations to all of our 2025 APAMSA Research Award winners!
Be sure to stay tuned for more opportunities to feature your research at upcoming regional and national conferences.
Interested in featuring your research with APAMSA? Email research@apamsa.org for more information!
Research Award Winners
Anne Chen – Impact of a Community Stroke Education Initiative for the Nashville Asian American and Pacific Islander Population
Background: Prior studies demonstrate an increased prevalence of primary intracranial hemorrhage with lengthened hospital stays within the Asian American and Pacific Islander (AAPI) population. AAPI patients who experience acute ischemic strokes may be less likely to receive intravenous thrombolytic therapy despite presenting with strokes of greater severity.[1] Yet, minimal research has been conducted to explore why these disparities exist. This project was conducted to assess for gaps within stroke education (symptom identification, risk factors, and primary prevention measures) and evaluate the utility of a stroke outreach initiative in the Nashville AAPI community.
Methods: A stroke outreach initiative was designed and administered to provide education on stroke symptoms using the FAST acronym, risk factors, and the importance of regular follow-up with primary care. Participants also received stroke educational materials in English, Simplified Chinese, Japanese, Korean, or Vietnamese from reliable sources (e.g., the American Heart Association, MedlinePlus). Pre- and post-education surveys assessed knowledge of stroke symptoms and primary stroke prevention. Proportional analysis and non-parametric analysis of paired comparisons (McNemar test) are reported.
Results: Twenty-two API community members at an AAPI festival in Nashville, TN participated in the initiative. Pre-initiative surveys revealed 8/22 (36%) participants were unable to identify stroke symptoms, 9/22 (40%) participants did not know what actions to take if someone is experiencing a stroke, and 10/22 (45%) participants did not follow up with primary care at least yearly (Figure 1). Post-initiative surveys showed a statistically significant improvement (p<0.05) where 21/22 (95%) participants correctly reported two of the FAST symptoms (Figure 2). 8/8 (100%) participants who previously were unable to identify stroke symptoms identified at least two symptoms post-initiative. All participants found this initiative beneficial.
Conclusion: An education initiative reviewing FAST symptoms, stroke risk factors, and primary stroke prevention through regular follow-up with primary care can improve the quality of stroke education in the Nashville AAPI population. Additional instruction and increased frequency of the initiative may improve retention of knowledge and further encourage stroke awareness and primary stroke prevention to a wider AAPI audience.
Alice Liu – Achieving Health Equity: Recognizing the Health Profiles of Asian American and Pacific Islander (AAPI) Communities in the Greater Cleveland Area and Closing the Gap in Clinical Trials
Background: Despite clinical trials playing a crucial role in treatment development, there is significant misalignment of minority race distribution between general population and clinical trial participants in the United States. Asian Americans are one of the most underrepresented minority groups-despite being the fastest-growing population in America-constituting less than 2% of clinical trial participants. This disparity affects the generalizability of clinical trial results and equitable healthcare delivery. The aim of this study is to identify barriers to clinical trial participation specific to AAPI communities in Greater Cleveland.
Methods: This research employs a mixed-methods approach to investigate cultural and socioeconomic barriers within AAPI communities. A survey encompassing cultural and socioeconomic barriers identified in previous literature were distributed to 50 participants in each of the following communities: Chinese (Cleveland Asiatown), Chinese (Greater Cleveland Area), Filipino, Pakistani and Afghan. Qualitative data was collected through focus groups, each comprising five community members from the groups mentioned above, to facilitate comprehensive exploration of distinct obstacles experienced by each community.
Results: We collected 196 surveys, with ages of participants ranging from 19 to 89 years old. 58% of participants have heard of clinical trials, but the vast majority (92%) knew nothing or little about them. 15% have participated or knew someone who participated in a clinical trial, though 48% said they are somewhat or very likely to participate if asked. The importance of incentives such as monetary compensation, transportation, and encouragement from trusted individuals varied widely between the communities. In the focus groups, specific groups noted unique challenges stemming from cultural and religious attitudes. Key takeaways included the importance of culturally competent outreach, transparent risk disclosure and education on the benefits of clinical trials to individuals and society, and community-centered approaches to recruitment.
Conclusions: While our findings mostly align with existing literature on the common barriers to clinical trial participation for minority populations, we highlight distinct barriers and motivators within various AAPI subgroups. Further meta-analysis of demographics data and health attitudes can be used to target and address AAPI clinical trial recruitment in the Greater Cleveland area.
Sunshine Liu – Understanding Diabetes: A Comparative Analysis of Diabetes Literacy and Confidence in South Asian and White Populations in Michigan
Background: Diabetes Mellitus (DM) prevention and management remains a challenge in Michigan. As of 2023, nearly half of the state’s population is affected with DM or pre-diabetes, with higher morbidity among minority groups. To address these disparities, osteopathic medical students at Michigan State University College of Osteopathic Medicine (MSUCOM), under faculty mentorship, created Understanding Diabetes, an educational project emphasizing biomedical understanding of DM and tailored management strategies. Initially piloted in the South Asian (SA) community in Oakland County MI, it expanded to Berrien County MI, an area with higher poverty and lower educational attainment. This enabled comparisons of objective understanding and subjective confidence in managing DM between White populations of lower socioeconomic status (SES) and SA populations of higher SES.
Methods: Understanding Diabetes used an observational descriptive study design (IRB STUDY00010026), in SA (N=18) and White (N=17) populations in selected geographic areas in Michigan. Data were collected to assess the baseline objective understanding of DM across several categories as well as participant-reported confidence in managing DM. Results were analyzed by comparing populations’ proportion of correct and affirmative responses using chi-squared proportion tests (CI95).
Results: SA participants reported significantly higher confidence overall in managing DM than White participants (74% vs 51%, p<0.05). This was also seen in categories of general knowledge (86% vs 56%, p<0.05), lifestyle management (81% vs 60%, p<0.05), and complications and emergency management (68% vs 47%, p<0.05). However, regarding objective understanding, no statistically significant differences were observed between the two populations (56% vs 58%).
Conclusion: SA participants exhibited similar levels of objective understanding of DM compared to White participants despite higher SES and greater educational attainment. These findings suggest that racial factors, such as language barriers and discrimination, may influence health literacy, potentially overriding SES and education. Additionally, the higher confidence reported by SA participants may reflect underlying cultural attitudes towards DM, including stigma and tendency to act on social desirability bias. As Michigan’s SA population grows, culturally sensitive educational interventions are critical to addressing disparities and improving outcomes in this at-risk population.
Nagasriya Ramisetty – Adaptation of the Health Stigma and Discrimination Framework for Asian American Mental Health Stigma and Reported Impact on Help-Seeking Behaviors
Background: Asian Americans face the highest mental health support need of any ethnic group in the United States, but the community reports severe underutilization of available mental healthcare services. Cultural differences are a major factor that contribute to differences in the help-seeking behaviors of Asian Americans, and researchers need to delineate the unique needs of this community to adapt and establish more culturally sensitive resources and outreach methods.
Methods: We conducted a comprehensive narrative review of the Google Scholar database for research studies (n=19) that inform the relationship between Asian American mental health and different dimensions of the Health Stigma and Discrimination (HSD) Framework – drivers and facilitators of stigma, manifestations of stigma experiences and practices, outcomes for affected populations and organizations, and the health and social impacts. The HSD framework has the potential to navigate the nuances of mental healthcare need for Asian Americans as a global cross-cutting measure that identifies the various facets of health stigma and impacts on public health outreach and interventions in marginalized communities. This framework critically moves away from the binary of the “stigmatized” and “stigmatizer”, and instead identifies how stigma detrimentally affects the health outcomes of the community at large.
Results: Studies (Table 1) found that Asian Americans’ evaluation of personal mental health need fell outside of the Western model of mental health understanding, resulting in lower service usage rates despite awareness of them. Major factors affecting help-seeking behavior included fear of social judgement, different manifestations of and language regarding mental distress, shame, familial pressure, and, unique to the Asian American community, expectations of success without struggle due to internalization of the model minority myth (Figure 1).
Conclusions: This evidence defends the need for culturally sensitive mental healthcare resources that acknowledge and dismantle the internal, perceived, and experienced stigma for members of the Asian American community. We are conducting semi-structured interviews with community members and healthcare providers to better understand representations of mental distress and identify the specific barriers that limit resource usage. Future research can be applied to tailoring existing resources and outreach to improve mental health outcomes for Asian Americans.
Shivam Bhargava – Evaluating the Impact of Social Support in South Asians and Arabs with Type 2 Diabetes Through a Family-Centered Diabetes Education Program
Background: Diabetes is the fourth leading cause of death among Asians in Chicago, and the top leading cause of death among Asian Indians. Limited research investigates the role that social support plays in South Asians with Type 2 Diabetes. The All One Community Program is a diabetes management program tailored toward South Asian and Arab communities with social support aspects, adapted from existing evidence-based curricula. The program is led by Asian Health Coalition in Chicago in collaboration with three different community-based organizations that serve South Asian and Arab immigrant communities.
Materials and Methods: The program is culturally and linguistically tailored for the South Asian and Arab community and includes health literacy components related to nutrition, stress, and exercise. The program includes 13 educational sessions that are held one hour per week. Biometric data (blood pressure, BMI, and A1c) is collected at baseline, 3-months, 6-months, and 9-months. Since the launch of the program in 2022, 142 individuals have been enrolled with 87 individuals being diagnosed with Type 2 Diabetes. A survey is administered at baseline, 6-months, and 9-months that contain questions about social support related to exercise, eating, and family/friends. Social support strategies include one on one weekly check-ins with CHWs, monthly webinars with healthcare professionals, and an interactive WhatsApp group for participants to interact and support each other outside of class.
Results: 54% of participants increased their overall social support scores from the start of the program to the end 9 months later. 67% of diabetic participants increased their social support for exercise score from baseline to 9 months. Social support for eating scores increased by an average of 5.3 points for participants from baseline to 9 months. 54% of participants increased the number of days they were physically active during the week from baseline to 9 months. A total of 98.8 pounds were lost among participants from baseline to 9 months.
Conclusion: The data analyzed informs attendees about the key roles that family members, community health workers, and additional support systems play in the management of diabetes. The research also highlights that when individuals have their family members or other support system members making the same lifestyle changes that they are, it positively impacts their motivation, behavior, and habits related to their type 2 diabetes.
Elizabeth Nguyen – Asians Be Checked: Uncovering Knowledge Deficits for Hepatitis B Among Vietnamese and Filipinos in South Texas
Background: Asian Americans are disproportionately at high risk for chronic hepatitis B virus (HBV) infection. In 2021, the CDC reported that although Asian Americans comprise only 6% of the US population, they make up 60% of chronic HBV cases and are nine times more likely to die from HBV-related complications than Caucasians. Hence, we created a community advocacy project to address this disparity by providing education and promoting screening to the Asian American community.
Our community assessments reveal that among South Texas Vietnamese, over 88% reported having never been screened or being unaware of their screening status. Subsequent assessments among Chinese and Korean communities showed that over 44% of participants have never been screened for HBV. These statistics highlight disparities in hepatitis B awareness. In 2023, the CDC updated its guidelines to include universal HBV screening, emphasizing the need to bridge gaps in care. The aim of this study is to engage stakeholders by evaluating understanding of HBV among the Vietnamese and Filipinos in South Texas.
Methods: Students volunteered with Vietnamese (Lien Hoa Buddhist Temple and Vietnamese Martyrs Church) and Filipino (Philippine American Chamber of Commerce and Filipino and Pacific Islander Festival) community partners at local events. Participants responded to an online survey with the questions: 1) Are Asian Americans at higher risk for hepatitis and liver cancer? 2) Do you know what hepatitis B is? 3) Is hepatitis B preventable? 4) Is hepatitis B treatable? 5) Have you ever been screened for hepatitis B? 6) Are you interested in being screened for hepatitis B? The responses formed the basis of the education talking points, and informational flyers (Figure 1) summarizing HBV education were provided. The collected data were analyzed for descriptive statistics.
Results: Most participants (59%, n=87) did not know that Asian Americans are at higher risk for HBV. 41% lacked awareness of HBV itself and 60% were unfamiliar with chronic HBV complications, such as liver disease and cancer. 53% did not know HBV is preventable and treatable. After learning about the vaccine, 66% expressed interest in learning more and getting screened.
Conclusions: The low HBV health literacy among Vietnamese and Filipino participants underscores the need for more outreach and education. Their strong interest in screening emphasizes the importance of providing these services to address this disparity.
Eugene Oh and Hayoung Anh – Addressing Bias and Advancing Equity for AANHPI Communities in Healthcare
Background: Racism, discrimination, and bias against Asian American and Pacific Islander (AAPI) individuals persist in healthcare, creating barriers to career advancement and impacting well-being1. Despite progress in equity, diversity, and inclusion (EDI), AAPI healthcare workers face unique challenges such as being perceived as submissive, which excludes them from leadership opportunities2. At UCLA Health, concerns from AAPI community members prompted surveys to assess these issues and develop actionable solutions.
Materials & Methods: Two Qualtrics surveys were distributed to the AAPI community at UCLA Health: the first in Oct-Nov 2022 (N=127) and the second in Dec 2023-Feb 2024 (N=106). Respondents included faculty (69%), medical students (21%), staff (6%), and residents/fellows (3%). The surveys assessed experiences of racism, discrimination, and bias, and perceptions of UCLA’s response.
Results: Key findings from the 2023 survey revealed that 74% of respondents witnessed racism, discrimination, or bias against AAPI individuals (vs. 70% in 2022), and 71% personally experienced such incidents (vs. 60% in 2022). Common forms of bias included implicit bias (witnessed by 89%, experienced by 84%) and microaggressions (witnessed by 82%, experienced by 64%). Negative impacts on well-being increased to 55% (vs. 38% in 2022), and 32% considered leaving UCLA due to these experiences. Only 41% felt UCLA addressed bias effectively, and 27% felt leadership was sufficiently educated on AAPI-specific issues.
Conclusions: Despite ongoing EDI efforts, these findings highlight persistent challenges and a critical need for AAPI-specific initiatives to address bias and promote inclusion in healthcare. In response, UCLA Health has taken meaningful steps, including the recent launch of the DGSOM Center for Asian Equity and Health, which provides training for faculty, staff, and students, fosters junior faculty leadership, and lays a foundation for a supportive environment and research. A coalition of faculty and trainees is also capturing real-life stories of discrimination to create a training video raising awareness and addressing AAPI racism, now in its final stages with plans for widespread distribution. These efforts underscore the importance of systemic interventions—by implementing targeted training, encouraging open conversations, and uniting the AAPI community, academic institutions can create environments where AAPI individuals feel supported, valued, and empowered.
Anthony Trieu, Joyce Xiong, and Joanna Sung – Primary Asian Language and Risk of Hepatic Complications in Asian Americans with Chronic Hepatitis B: A Retrospective Cohort Study
Background: Chronic hepatitis B (CHB) affects Asian Americans disproportionately, yet the role of language proficiency in health outcomes remains understudied.1-2 Limited English proficiency may contribute to varied outcomes through healthcare access, communication, and treatment adherence barriers.3-4 This study investigates the impact of Asian primary language preferences on adverse outcomes in Asian Americans with CHB.
Methods: Using the TriNetX platform, we conducted a retrospective cohort study of Asian American patients diagnosed with CHB (ICD-10: B18.1), excluding those with co-infection by the hepatitis D virus (ICD-10: B18.2) and Type 2 diabetes (ICD-10: E11). Patients were stratified into two cohorts based on primary language preference: English vs. certain Asian languages (Vietnamese, Korean, or Chinese). 10-year risk of key adverse outcomes, including liver cell carcinoma (ICD-10: C22.0), fibrosis and cirrhosis of liver (ICD-10: K74), liver transplant status (ICD-10: Z94.4) and portal hypertension (ICD-10: K76.6) were analyzed across language groups. Propensity score matching was used to adjust for age and gender. Certain social factors and laboratory values to assess the severity of hepatitis could not be accounted for due to limitations to available data.
Results: Preliminary findings revealed differences in adverse outcomes based on language preference. Chinese-speaking patients demonstrated a decreased risk of adverse outcomes compared to their English-speaking counterparts, specifically in liver transplant status, cirrhosis, and portal hypertension. Vietnamese- and Korean-speaking patients exhibited a significantly higher risk of liver cell carcinoma. However, no significant differences were observed in liver transplant status, portal hypertension, or cirrhosis. Differences persisted after propensity score matching.
Conclusions: Our findings suggest that primary language preference may influence health outcomes in Asian Americans with CHB. Factors such as varied disease management education in non-English languages, cultural awareness, and public health programs domestically and/or countries of origin may contribute to different outcomes for certain groups.5-7 Future studies may explore the intersection of language proficiency, social support, and socioeconomic factors to better address disparities in CHB outcomes.
Avni Varshneya – Health Education as Harm Reduction for Clients in Addiction Recovery
Background: First Step Home (FSH) is an addiction treatment facility for people who identify as women recovering from substance use disorder (SUD). Higher levels of health knowledge and literacy can increase quality of life and mental health in this community. FSH was seeking to empower their clients through health education and learn more about the impact of a new adulterant, xylazine.
Materials and Methods: A 15-session educational course was conducted on sexual/mental health, nutrition/exercise, xylazine/harm reduction, and wound care/first aid. Pre and post-session quizzes were analyzed with a Wilcoxon signed-rank t-test to assess knowledge improvement. Gathered client feedback on health education sessions. Distributed a qualitative and quantitative survey to determine how xylazine impacts FSH residents.
Results: An average 14% increase in post-quizzes compared to the pre-quizzes was found (σ = .100, n = 8). The session on wound care and first aid showed a statistically significant improvement of 27% (p = .0312, σ = .163). Through the xylazine impact study, 28 clients were surveyed. One-third of women reported being impacted by xylazine or knowing someone else who was impacted. 50% of the clients surveyed did not know what xylazine was, and 89.3% did not know the effects of xylazine on the body or how to take care of xylazine wounds.
Conclusion: Women reported being empowered to make decisions about their healthcare and schedule reproductive health screenings after the educational course. More participants are needed to demonstrate a significant link between health education improving health knowledge for women undergoing SUD treatment. Wound care and first aid sessions showed significant increases in scores. These skills should continue to be taught because they are vital to saving the lives of people with SUD. The results of the xylazine impact survey show a striking lack of awareness about xylazine amongst clients. If clients did know what xylazine was, they often did not know about wound care or how the drug affected the body. Notably, some clients had healed wounds and only realized they may be due to xylazine as they were taking the survey. These results indicate more education is needed to equip women in addiction recovery with knowledge about harmful adulterants like xylazine, and empower them with sessions on first aid, harm reduction, and wound care techniques.
Gabriella Tran – Investigating Quality of Life Measures in Birdshot Chorioretinopathy
Background: Birdshot chorioretinopathy (BSCR) is a chronic posterior uveitis that can significantly impact visual function. Patient-reported outcomes (PROs) have gained importance in evaluating the impact of patients’ perceptions of their quality of life. This study aimed to investigate the use of psychometrically validated PRO measures, the Michigan Retinal Degeneration Questionnaire (MRDQ) and Michigan Vision-related Anxiety Questionnaire (MVAQ), for BSCR patients.
Methods: A dual-center mixed method observational study was conducted on patients with BSCR (n=21). The MRDQ and MVAQ were administered to these patients, and retrospective chart review was performed. Graded response models were fit by Cai’s Metropolis-Hastings Robbins-Monro algorithm using the R (version 3.6.3) package mirtscores for seven parameters from the MRDQ. These scores were then compared with the presence or absence of retinal vasculitis and the time between diagnosis and the most recent follow-up.
Results: Analysis of the MRDQ parameters revealed previously unrecognized patterns in visual function among birdshot chorioretinopathy (BSCR) patients. Photosensitivity with a value of 0.73 ± 1.3 and color vision with a value of 0.66 ± 0.11 were the highest scoring domains. The lowest scoring domains were mesopic peripheral function at 0.059 ± 0.09 and scotopic function 0.082 ± 0.10. A trend of retinal vasculitis impacting color vision and photosensitivity was observed. Interestingly, a significant correlation between time from diagnosis to most recent follow-up being ≥5 years and decreased photosensitivity was observed (p=0.017). MVAQ showed higher anxiety due to cone dysfunction scores, compared to rod dysfunction, further supporting that color vision is one of the most greatly impacted domains for birdshot patients.
Conclusions: The MRDQ/MVAQ results provide a previously unrecognized feature of birdshot, which is a significant impact on color vision. The domains most affected in BSCR are notably different from those reported in retinitis pigmentosa (RP). In RP, the highest observed MRDQ scores were mesopic peripheral function and contrast sensitivity, while the lowest were in photosensitivity and color vision. Both RP and BSCR affect photoreceptors, but these results indicate potential differences in pathophysiologic processes.
Hanna Suh, Sophie Lu – Investigating the Health Needs of Asiatown Community Members in Cleveland, Ohio
Background: The Asian and Pacific Islander community comprise 2.5% of Cleveland’s and 3.5% of Cuyahoga county’s population according to the 2020 census. The health needs of this community, however, are not well characterized. The aim of this study was to assess the subjective factors that affect health needs and outcomes, self-efficacy, and healthcare interactions among Cleveland’s Asiatown members.
Methods: We administered a survey to Asiatown members asking about barriers to healthcare, health literacy and transportation. Surveys were provided in English, simplified Chinese, traditional Chinese, and Korean. Responses were collected in-person at community health outreach events and online via Qualtrics. Data analyses, including t-tests with unequal variances and Fisher’s exact tests were conducted in R.
Results: We enrolled 78 participants with a mean age of 72, of which there were 60 females and 14 males (4 NA). Self-reported race was 77 Asians and 1 mixed race, with 74 Chinese, 4 Koreans, and 1 White/Chinese. The top two health concerns were blood pressure and diabetes with 36 and 19 votes respectively. 75 participants (96%) had health insurance. Most participants either drove themselves (37.2%) or were driven by others (24.4%). The primary mode of transportation of participants ages 65 and older was significantly different from those younger than 65 (p=0.002). While both groups reported driving themselves, those aged 65 and older were driven by others more often. Regarding time spent traveling to health care visits, most participants spent 10-30 minutes. Lastly, 53.8% of participants said they go to health appointments alone versus 41% who go with others (4 NA). There were no significant differences in responses based on sex.
Conclusions: Our results suggest unmet health needs of a population of elderly community members who live in Asiatown. While participants tend to have health insurance, there appear to be other barriers to health care, such as transportation insecurity and lack of social support. Limitations of this study include a small sample size as well as limited literacy in their primary language among some participants which may bias results. Future directions include tailoring future health fairs and volunteer programs to address the gaps identified in this study, such as providing transportation support.
Hao Chen – Reassessing the Healthy Immigrant Effect: Elevated Chronic Disease Prevalence Among Asian Immigrants Compared to U.S.-Born Asians
Introduction: The “healthy immigrant effect” suggests that immigrants often have better health outcomes than their native-born counterparts. This study reevaluates this concept by analyzing the prevalence of chronic diseases among Asian immigrants compared to U.S.-born Asian Americans and examining healthcare access metrics to explore potential contributors to health disparities.
Methods: Data from the Integrated Public Use Microdata Series (IPUMS) National Health Interview Survey (NHIS) was used to analyze to assess the prevalence of hypercholesterolemia, hypertension, diabetes mellitus, and cancer among individuals aged 18 and older. Foreign-born Asian immigrants were categorized by U.S. residency duration: less than one year, 1–less than 5 years, 5– less than 10 years, and more than 15 years. Healthcare access metrics, including health insurance coverage, recent doctor visits, and having a usual place of care, were also evaluated. Weighted percentages and chi-square tests were used to identify differences in prevalence and access.
Results: Among Asian immigrants, hypercholesterolemia and hypertension prevalence initially declined with longer residency—from 25.0% and 16.8% (less than one year) to 16.7% and 10.8% (5– less than 10 years)—but rose to 36.7% for both conditions after 15 years. Similarly, cancer and diabetes prevalence were 0% (less than one year), fluctuating between 1 and 15 years, and 4.6% and 15.2%, for over 15 years, respectively.
Healthcare access improved with residency duration, with insurance coverage rising from 86.3% to 97.8%, and having a usual place of care increasing from 42.6% to 91.5%. However, recent doctor visits declined (89.3% to 85.5%). Compared to U.S.-born Asians, foreign-born Asian immigrants reported higher prevalence of chronic conditions, including cancer (3.9% vs. 2.4%), hypercholesterolemia (30.6% vs. 19.6%), hypertension (29.3% vs. 16.7%), and diabetes (12.4% vs. 3.9%).
Conclusion: This study challenges the “healthy immigrant effect,” showing higher chronic disease prevalence among foreign-born Asian immigrants than U.S.-born Asians, including recent arrivals. These disparities are unlikely driven by socioeconomic barriers, as healthcare access metrics were comparable. Potential contributors include language barriers, acculturation stress, pre-existing conditions, or lifestyle changes. Future research should explore these disparities’ underlying causes and guide targeted interventions.
Himi Begum – Cervical Cancer Incidence Patterns Across Asian and Pacific Islander Populations in the U.S. (2004–2021)
Background: Cervical cancer remains a major public health issue, with significant differences in diagnosis and survival rates across racial and ethnic groups. Non-Hispanic Asian/Pacific Islander (NHAPI) women represent a diverse population, with unique challenges in accessing care and timely diagnosis. This poses a significant public health problem, given that cancer is the leading cause of death among Asian American women. This study aims to examine disparities in cervical cancer stage at diagnosis and incidence rates among API women, utilizing Surveillance, Epidemiology, and End Results (SEER) data from 2004 to 2021.
Materials and Methods: We conducted a retrospective analysis of cervical cancer cases recorded in the SEER*Stat database from 2004 to 2021. Data were stratified by race and ethnicity, focusing on specific NHAPI subgroups (e.g., Vietnamese, Korean, Japanese, Chinese, Filipino). We compared stage at diagnosis (i.e., Localized, Regional, Distant), age-adjusted incidence rates, and mortality rates between NHAPI subgroups and non-Hispanic White women.
Results: Overall, the 5-year cervical cancer incidence rates for NHAPI women were generally lower than those for non-Hispanic White women, except for Native Hawaiian women (6.1 per 100,000 vs. 6.9 per 100,000). The 5-year age-adjusted mortality rates were lower for NHAPI women compared to non-Hispanic White women (1.6 per 100,000 vs. 2.1 per 100,000). In general, certain API groups had less favorable distributions of stage at diagnosis compared to non-Hispanic White women. Among stratified NHAPI subgroups, Chinese and Filipino women had the highest rates of late-stage cervical cancer diagnoses.
Conclusions: This study highlights disparities in cervical cancer incidence and stage at diagnosis between specific NHAPI subgroups and non-Hispanic White women. The higher rates of late-stage diagnoses among Chinese and Filipino women underscore the need for targeted cancer prevention measures. These findings demonstrate the importance of understanding the unique health challenges across NHAPI groups to improve outcomes.
Isabel Kilroy – Built Environment and Housing Quality on Mental Health Outcomes Among Filipinos in the HoPES Cohort
Background: The rising prevalence of mental health issues is a global public health concern. A social determinants approach to mental health highlights that the conditions in which individuals live, work, and grow shape mental health outcomes. Housing is a cardinal social determinant of health, and recent research has emphasized the impact of the built environment (including housing quality and urban design) on well-being. The Philippines, ranked third in mental illness prevalence in the Western Pacific, faces a housing crisis worsened by socioeconomic inequality and climate disaster. Thus, exploring the impact of the built environment on Filipino mental health is crucial. Filipino Americans comprise the 3rd largest Asian ethnic subgroup in the U.S., and Asians are projected to be the largest immigrant group in the U.S. by 2055. Within this community, mental health stigma and cultural values often discourage formal help-seeking, despite high rates of psychological distress. Therefore, identifying “upstream factors” such as housing and the built environment is critical to addressing the mental health needs of Filipino Americans and AANHPI more broadly. Materials and
Methods: We conducted a secondary analysis of baseline data from the non-migrant sample of the Health of Philippine Emigrants Study (HoPES; n=805). Using multiple linear regression and logistic regression analyses, we examined the association between built environment quality and depressive symptoms, and the impact of built environment quality on substance use, specifically cigarette use and binge drinking.
Results: Overall, poor quality built environment was significantly associated with greater depressive symptoms (β = 0.079, p = 0.013) and smoking (β = 0.13, p = 0.0013), but not binge drinking (β = -0.058, p = 0.115) after adjusting for covariates.
Conclusion: Clinicians across all specialties play a key role in recognizing the impact of housing quality and the built environment on mental health. Integrating this awareness into medical training, incorporating questions on built environment within clinical assessment, and fostering interdisciplinary collaboration, especially with public health and social work fields, are essential steps to addressing the impact of built environment on mental health outcomes in the Filipino community. Ultimately, advocating for healthier policies that improve the conditions in which patients live, work, and grow is vital to optimizing community health outcomes.
Rachel Prince – The Role of Asian Culture and Language in Diabetes and Vision Care
Background: Asians face high rates of diabetes and diabetic retinopathy (DR) and have disproportionately low diabetes screening rates but are underrepresented in vision research, with distinct ethnicities often aggregated. We investigated the role of language and cultural preferences in shaping the understanding and management of diabetes and eye care by analyzing perspectives across Asian subgroups.
Methods: We conducted virtual semi-structured interviews with a purposive sample of Asian-identifying, English-speaking adults with diabetes residing in Connecticut. We created an interview guide based on our DR determinants framework. All interviews were transcribed and analyzed using NVivo software. We conducted consensus-based coding and both deductive and inductive thematic analysis until we achieved thematic saturation.
Results: We recruited 10 participants with diabetes (median age 65.9 years, 60% female) of Chinese, Filipino, Indian, and Vietnamese ethnicities. We identified 27 concepts under eight themes: cues to action, cultural understanding, diabetes management, health awareness, knowledge-creating experiences, patient education, physician-patient interaction, and vision status. Over half the participants stated they were not made aware of the link between eye health and diabetes or the rationale behind diabetic eye exams. Participants preferred providers of similar ethnicities due to a shared understanding of diet, lifestyle, and language, which improved comprehension and management of their health conditions. They also cited diet, lifestyle, and cultural beliefs as key challenges of managing diabetes, emphasizing the need for cultural integration into health management plans. Participants also generated ideas for improved communication with patients with limited English proficiency. While the original framework examined broad factors influencing DR screening, our study focused on cultural and linguistic influences on diabetes and eye health in Asians.
Conclusions: Participants recognize the need for cultural understanding from providers, especially in regard to patient education and diabetes management. It is crucial to develop interventions tailored to Asian communities that emphasize the link between diabetes and eye health and address cultural and language barriers.
Sandhya Sewnauth – The Impact of Colonialism on Present-Day Indo-Caribbean Health
Background: Indo-Caribbeans are currently the fifth largest immigrant group in New York City, and the second largest immigrant population in the borough of Queens. There are several significant health disparities that exist within this community, including elevated rates of cardiovascular disease, diabetes, and binge drinking. To develop culturally appropriate and trauma-informed strategies to address this, we need to understand the complex historical factors that led to disproportionate health outcomes. By analyzing colonialism as a social determinant of health, we can create sustainable healthcare improvements within this under-researched population of the South Asian diaspora.
Methods: Existing literature on present-day health disparities was assessed using PubMed and Research Open World databases. A community health resources and needs assessment conducted by the NYU Center for the Study of Asian American Health from 2013-2015 was also consulted. Primary sources from the colonial period were accessed at the British Library in London, UK.
Results: The Indian indenture system contributed to several health disparities in the Indo-Caribbean population. This includes the cardiometabolic effects of colonial-driven famines that devastated the regions of India where the majority of indentured laborers were recruited. The economy in the Caribbean colonies focused solely on sugar cultivation, which influenced the diet and lifestyle of this population, including the high number of distilleries in their communities. The experiences of working as indentured laborers also led to mental health crises, including suicidal ideation, and generational trauma among the diaspora.
Conclusions: The health of Indo-Caribbean immigrants is uniquely affected by the legacy of the indentured laborer system during British colonial rule. These results will inform a culturally appropriate and trauma-informed resource guide that focuses on the topics of cardiovascular disease, diabetes, alcohol use disorder, and mental health. While more research is needed on present-day health disparities within this population, tailored resource guides will empower community members to tackle negative health outcomes, enabling future generations to thrive.
Arion Yu – The acute effects of alpha-lactalbumin intake on tryptophan metabolites and mood in older adults with Mild Cognitive Impairment
Background: Mild Cognitive Impairment (MCI) represents a transitional stage between normal cognitive aging and more severe neurodegenerative disorders in the elderly such as Alzheimer’s Disease. MCI is often accompanied by depressed mood and other mood disturbances which can obfuscate what is causing declining cognition. Serotonin (5-HT), a neurotransmitter involved in regulating mood, is synthesized from the essential amino acid tryptophan. Availability of serotonin is largely influenced by the metabolism of tryptophan through either the serotonin or kynurenine pathway. This manuscript explores the potential relationship between MCI, depressed mood, and tryptophan metabolism in the elderly, with a particular focus on the effects of a tryptophan-rich dietary intervention. We first examine the differences in tryptophan metabolism between MCI elderly adults and healthy older adults at baseline. Subsequently, we examine how intake of alpha-lactalbumin (ALAC), a protein rich in tryptophan, affects tryptophan metabolism and if it could serve as an effective strategy for enhancing mood in older adults with mild cognitive impairment.
Methods: 32 older adults (age 55 and up) with MCI and 26 older adults matched for age, sex, and BMI without MCI participated in this cross sectional study. Serum tryptophan metabolites at baseline were measured. A smaller subset of these subjects then consumed a meal enriched with ALAC. Plasma tryptophan metabolites after introduction of the meal were measured and changes in mood were assessed before and after meal intake.
Results: MCI subjects had higher levels of plasma anthranilic acid at baseline. Intake of ALAC resulted in an increase in plasma tryptophan (TRP), kynurenine (KYN) , 3-hydroxykynurenine (3-HK), anthranilic acid (AA), kynurenic acid (KYNA), and picolinic acid (PICO). There were no differences in 5-HT before and after ALAC intake. Additionally, there was a MCI interaction with picolinic acid. The TRP/LNAA ratio increased by 89.9% in MCI subjects and 95.9% in controls. There were no acute changes in mood before and after ALAC intake.
Conclusions: Elderly adults with MCI have different tryptophan metabolism down the kynurenine pathway. Consumption of a dietary protein rich in tryptophan increases metabolites of the kynurenine pathway as well as the TRP/LNAA ratio. The ALAC protein had no effect on mood.
Brandon Deguzman – Underdiagnosis of Trauma and PTSD in a Low-Income, Minority-Predominant Outpatient Setting: A Comparison of Self-Assessments and Medical Records
Background: Posttraumatic stress disorder (PTSD) is a debilitating psychiatric condition that can result from traumatic events. It is characterized by intrusive thoughts, avoidance, and mood changes, and often complicated by several common comorbidities, including major depression and substance use disorders. PTSD has a lifetime prevalence of 9.4% in the United States but is often under- or mis-diagnosed. Several validated screening tools and structured assessments exist to detect trauma and PTSD, but their efficacy has not been well studied in low income, inner-city outpatient settings, in which trauma tends to be highly prevalent. The current study evaluated if validated self-report measures would capture the prevalence and trauma elements of PTSD more accurately than standard clinical interviews. The study characterized the demographics of an inner-city outpatient population, PTSD prevalence, comorbidities, and treatment.
Materials and Methods: A survey was conducted of 100 adult outpatients being treated at a large inner-city psychiatric clinic. This clinic provides safety-net services for an otherwise unserved, mostly minority population in Los Angeles County. Each participant completed two self-report measures: Life Events Checklist for DSM-5-Extended (LEC-5) and the PTSD Checklist for DSM-5 (PCL-5). Patient responses to the measures were then compared to corresponding data extracted from a medical chart review.
Results: Of the 100 participants, 50 were male, 50 were female, 66 self-identified as Latine/x, and 79 were unmarried. Physical assault (60%), transportation accidents (57%), and other unwanted sexual experiences (47%) were the most frequently reported traumas. The most commonly endorsed symptoms were feeling upset when reminded of the trauma (68%), insomnia (68%), and difficulty concentrating (66%). 56 participants met criteria for a provisional DSM-5 PTSD diagnosis, but only 29 indicated a PTSD diagnosis in their medical records. The PCL-5 and the medical record demonstrated fair agreement in PTSD diagnosis (Kappa = 0.219; SE of kappa = 0.082). A significant difference was found between the LEC-5 and the medical record in capturing the number of trauma event categories endorsed by participants (t(99) = 13.1834, p < .0001).
Conclusions: PTSD may be underdiagnosed in outpatient settings. Implementing validated self-report trauma screening measures may improve identification and treatment of PTSD among historically underserved populations.
John Huang – Evaluating Diurnal Responses to Timolol and Latanoprost from iCare HOME Intraocular Pressure Data
Background: Current glaucoma management relies on trial-and error with intraocular pressure (IOP) measured only during office hours. This limits our understanding of drug responses over a diurnal period. iCare HOME, a self-tonometer, may address this issue. This study examined timolol and latanoprost responders using diurnal IOP data from iCare HOME via cosinor rhythmometry.
Methods: Forty-seven subjects (22 male, mean age 61±9 years) with ocular hypertension or open-angle glaucoma, were enrolled in a randomized, crossover trial of latanoprost and timolol. IOP was measured using pneumatonometry and iCare IC200 at 3 of 6 study visits: baseline, after 1 week of first treatment, and after 1 week of second treatment. Subjects measured their IOP with iCare HOME at least 6 times daily for 1 week before visits. Eyes were labeled responders to timolol or latanoprost if IOP decreased ≥15% from baseline. Diurnal IOP data were analyzed and modeled with cosinor rhythmometry using R (Figure 1).
Results: For timolol, iCare HOME and pneumatonometry identified the same eye as a responder or non-responder in 60.4% of eyes (n=53). For latanoprost, the two tonometers agreed in 69.6% of eyes (n=56). Agreement between iCare HOME and iCare IC200 occurred in 54.5% of eyes (n=55) for timolol and 62.1% of eyes (n=58) for latanoprost (Figure 2). The chi-squared test for independence revealed that classifications of latanoprost responders between iCare HOME and the clinic tonometers, pneumatonometry (p=0.0025) and iCare IC200 (p=0.0137), were significantly different. No such difference was found with timolol responder classification.
Conclusions: When determining timolol responders, home and clinic tonometers show comparable classifications. For latanoprost, significant differences in classifications highlight discrepancies between home and clinic tonometry, suggesting that incorporating 24-hour monitoring may impact classifications. iCare HOME may improve glaucoma management by capturing IOP fluctuations to better identify responders.
Juben Angelo Saez – The angiotensin (1-7) glycopeptide PNA5 reduces cognitive dysfunction in a chronic progressive mouse model of Parkinson’s disease through modulation of neuroinflammation
Parkinson Disease (PD) is a widespread disease, however treatment primarily focuses on resolution of motor symptoms with currently no therapeutics that aim to accurately improve cognitive decline associated with PD. It has been shown in previous studies that MAS receptor agonism via glycosylated angiotensin (1-7) peptide, PNA5, effectively reduces cognitive decline in models of vascular contributions to cognitive impairment and dementia (VCID). The two goals of this study were to determine if systemic administration of PNA5 decreased cognitive decline in a PD mouse model and to determine if improved cognitive status can be correlated to histopathological or blood-plasma changes. Mice over-expressing human, wild-type α-synuclein (αSyn) under the Thy1 promoter (Thy1-αSyn- mice), were used as a model of PD with cognitive decline. Beginning at 4 months of age, Thy1-αSyn mice were treated with a systemic dose of PNA5 or saline solution (1 mg/kg/day). Thy1-αSyn mice then underwent behavioral testing at 6 months of age which included Y-maze, nest building, open field test, novel object recognition, and challenging beam test. Thy1-αSyn- mice were compared with wild-type mice treated with saline. Mice brains were then analyzed for changes to brain pathology using immunohistochemistry, microscopy and image analysis, stereology, Western blot, and plasma collection and immunoassay. Treatment with PNA5 reversed cognitive dysfunction measured by Novel Object Recognition and spontaneous alteration in a Y-maze in Thy1-αSyn mice. PNA5 treatment was specific to cognitive deficits as the number of errors per step on the challenging beam and nestlet building test did not change between Thy1-αSyn mice and WT. With analysis of brain tissue, enhanced cognition was associated with decreases in hippocampal inflammation and reductions in circulating levels of Macrophage Induced Protein (MIP-1β), a chemokine implicated in cognitive decline. Neuronal loss was also blunted within the CA3 hippocampal region of PNA5-treated αsyn mice. This data reveals that PNA5 treatment reduces cognitive dysfunction in a mouse model of PD and that MIP-1β can be used as a candidate biomarker for future target engagement.
Liana Ysabel Bautista – Pain Perception in Patients with Comorbid Fibromyalgia, ADHD and Obstructive Sleep Apnea Undergoing Treatment with Continuous Positive Airway Pressure: A Cross-Sectional Study
Background: Fibromyalgia (FM) is a syndrome of chronic widespread musculoskeletal pain with serious adverse health and economic outcomes (1,2). FM is not well understood, but ongoing research suggests that it is a disorder of pain regulation. It is specifically thought that central sensitization results in pain hypersensitivity. Patients experience chronic pain in the absence of musculoskeletal inflammation and structural damage (3). Moreover, there is a high frequency of ADHD symptoms and diagnosis among patients with FM, and improvement in sleep may improve not only pain but also executive function (4). For some patients with ADHD, symptoms are worsened by sleep disturbance due to OSA, and symptoms are markedly improved with appropriate treatment of obstructive sleep apnea (OSA) (5). Because sleep (and especially REM sleep) deprivation increases central sensitization, it stands to reason that for patients with FM and OSA, appropriate treatment of OSA will lead to improvement in pain perception and neuropsychiatric sequelae (5-9).
Aims: Examine the relationship of pain perception between three commonly comorbid disorders: Fibromyalgia (FM), Obstructive Sleep Apnea (OSA), and Attention Deficit/Hyperactivity Disorder (ADHD). We specifically aim to examine the effect of CPAP treatment on attention in patients with comorbid FM and OSA
Methods: After IRB approval, FM patients with OSA were identified. After written informed consent, ASRS-v1.1 was administered to FM patients seen at Loyola Outpatient center. McGill Pain Questionnaire (MPQ) 11 was administered. We analyzed sleep studies and divided the FM patients into 3 groups 1.Mild OSA 2. Moderate OSA 3. Severe OSA based on apnea/hypopnea index (AHI). We then identified OSA patients undergoing CPAP treatment and analyzed their ASRS score and compared ASRS score to non CPAP patients. REM rebound scores were analyzed.
Results: With MPQ of +25 signifying severe pain.
ADHD positive n = 24
ADHD positive and Severe MPQ Score n= 16 MPQ mean score ADHD positive: 27.67 ADHD CPAP Compliance: 44%
ADHD negative n = 26
ADHD positive and Severe MPQ Score n = 7 MPQ mean score ADHD negative: 19.23 ADHD CPAP Compliance: 55%
Conclusion: Findings show that there is a correlation between a positive ADHD diagnosis and having a more severe pain perception regarding FM symptoms. With regards to CPAP compliance, which could be influencing pain perception in these patients, we saw the ADHD positive group was less compliant.
Manav Jain – Assessment of Plasma Tetrahydrobiopterin (BH4) Levels in Individuals with Multiple Sclerosis: An Exploratory Study
Background: Multiple sclerosis (MS) is a complex neurological disease with varied clinical presentations. Oxidative stress is a key contributor to MS pathogenesis, characterized by the overproduction of reactive oxygen and nitrogen species, resulting in neurotoxicity and disease progression. Tetrahydrobiopterin (BH4), a cofactor for nitric oxide synthase, is vital for redox homeostasis. BH4 depletion amplifies oxidative stress, disrupting nitric oxide synthesis. Prior research indicates that reduced BH4 levels correlate with oxidative stress-related pathologies. This study investigates BH4 as a potential non-invasive biomarker for MS diagnosis, hypothesizing lower BH4 levels in MS patients compared to healthy controls.
Materials and Methods: This proof-of-concept study recruited MS patients (relapsing-remitting MS [RRMS], secondary-progressive MS [SPMS], primary-progressive MS [PPMS], and clinically isolated syndrome [CIS]) and healthy controls. Inclusion criteria were ages 18–40, BMI <28.5, ambulatory status (EDSS <3.5), and informed consent. Exclusions included significant systemic diseases, pregnancy, and recent smoking or medication use. Plasma BH4 levels were quantified via liquid chromatography-mass spectrometry (LC-MS). Stabilization agents included dithiothreitol, ascorbic acid, and trichloroacetic acid. Samples were centrifuged, snap-frozen, and stored at −80°C. Statistical analyses employed independent t-tests or Mann-Whitney U tests for non-normal data.
Results: Pilot data from 20 plasma samples revealed reduced BH4 levels in MS patients (6 ± 2 ng/mL) compared to controls (7.7 ± 2 ng/mL, p < 0.01, Cohen’s d). Reduced BH4 levels were observed in young, mobile RRMS patients with mild disability (EDSS <3.5), stable disease, no comorbidities, and no smoking or excessive alcohol use. Participants were predominantly on high-efficacy disease-modifying therapies.
Conclusions: Preliminary findings highlight BH4’s potential as a sensitive biomarker for oxidative stress in MS, independent of clinical stability or radiological findings. This study underscores the importance of integrating molecular biomarkers like BH4 with traditional markers (e.g., MRI, neurofilaments, GFAP) to enhance MS management and individualized treatment strategies. Ongoing recruitment aims to validate these findings across diverse MS phenotypes.
Charles Guo – Suppression of Integrin-Linked Kinase Inhibits SPARC’s Effect on Extracellular Matrix and Intraocular Pressure
Background: Primary open-angle glaucoma is a progressive eye disease where aqueous humor is inadequately drained from the trabecular meshwork (TM). While the exact mechanism is still unknown, Secreted Protein, Acidic and Rich in Cysteine (SPARC) is shown to be a key regulator of extracellular matrix (ECM) proteins that elevate intraocular pressure (IOP). Integrin-Linked Kinase (ILK) is a membrane-bound kinase shown to interact with SPARC and also regulate the ECM. We overexpressed SPARC and then inhibited ILK in mice and human models to investigate the pathway of how SPARC regulates ECM proteins in the trabecular meshwork (TM). We hypothesize that SPARC mediates its effect through ILK.
Materials and Methods: Live mice eyes, human cadaveric anterior segments, and primary human TM cells were treated with an adenovirus carrying cDNA of human SPARC (Ad.SPARC) causing overexpression and a lentivirus carrying shRNA targeting ILK (shILK) to inhibit ILK. IOP measurements were performed on live mice eyes and human anterior segments. TM cells were analyzed by immunoblotting and immunostaining. Statistical analysis was performed in Prism.
Results: SPARC overexpression in mice increased IOP compared to baseline by 1.61±0.94mmHg (p=0.047, n=10). Subsequent shRNA-mediated ILK inhibition reduced IOP by 3.51±0.92mmHg (p=0.009, n=8) compared to SPARC overexpression. In human anterior segments, SPARC overexpression elevated IOP 2.10±0.25fold (p=0.021, n=4), however, addition of shILK attenuated SPARC’s effect and decreased IOP 0.61±0.31fold (p=0.015, n=4). In human TM cells, SPARC overexpression increased levels 3.2±2.5fold (p=0.029, n=12) and also induced elevated laminin 1.45±0.37fold (p=0.004, n=10) compared to controls. ILK inhibition reduced levels 0.54±0.17fold (p<0.001, n=12) and also reduced levels of collagen I 0.60±0.17fold (p<0.001, n=8) and collagen VI 0.67±0.17fold (p<0.001, n=8).
Conclusions: ILK inhibition by shRNA attenuated the effects of SPARC overexpression on IOP and ECM proteins, implicating ILK signaling as a major molecular pathway of SPARC-mediated regulation of ECM homeostasis in TM. ILK is important in the downstream cascade of SPARC.
Dottie Yu – Development of Multiple Myeloma-on-a-Chip for Disease Modeling
Background: A hallmark of multiple myeloma (MM) is the transformation of the bone marrow (BM) microenvironment into an immunosuppressive niche that supports the migration, proliferation, and survival of malignant cells[1–3]. Preclinical murine models and 2D/3D cell culture systems are commonly used to study MM; however, they can be limited in fully capturing the complexity of the tumor microenvironment in a human context[4]. As such, there is a need for an ex-vivo model that most accurately recapitulates the immune and stromal components of the human BM environment, especially for testing CAR T-Cell therapy.
Materials and Methods: To emulate the microarchitecture of the BM, we designed the chip with concentric chambers representing the central sinus (central inlet), medullary cavity (inner chamber), and endosteal region (middle chamber) of the bone marrow. Chips are fabricated using replica molding technique by casting polydimethylsiloxane onto silicon wafer molds, followed by hole-punching inlets and outlets, bonding onto glass coverslips, and UV sterilization. To recreate the cellular composition of the BM, we seeded the chambers with human multiple myeloma blasts, primary human umbilical endothelial cells, primary human mesenchymal stem cells, osteoblasts, and fibroblasts. The chips were cultured for 1 week and characterized by immunostaining of vessel, immune and multiple myeloma markers.
Results: Our model demonstrated key features of the BM tissue in MM, with evidence of vascularization and MM cell localization in the medullary cavity region (inner chamber). Validation was further supported by integrating scRNA-seq data from 22115 healthy, new diagnosis, and relapse MM cells. We classified the cells into 8 immune cell types and found distinct changes in gene expression between the relapse samples compared to the healthy and new diagnosis ones. We are now investigating the role of these genes in MM progression and treatment resistance in CAR T-cell therapy using our MM-on-a-Chip.
Conclusion: The MM-on-a-Chip emulates key features of the BM environment in MM and provides a novel platform for studying the cellular interactions and microenvironment evolution in disease progression. Integrating this model with scRNA-seq analysis will build on our current understanding of the immune niche in MM progression and serve as a promising avenue for preclinical testing of novel therapies.
APAMSA Merchandise Order Form: Graduation Cords